| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website http://www.neurores.org |
Case Report
Volume 1, Number 2, June 2011, pages 74-77
Spinal Cord Sarcoidosis: An Unusual Cause of Neurogenic Bladder Dysfunction
Ali Chouaiba, c, Patrick Cabanisa, Thierry Billebauda, Meryeme EL Machkourb
aDepartment of Urology, Creteil’s Inter-Communal Hospital, Creteil, France
bDepartment of Neurology, Kremlin-Bicetre Hospital, APHP, Paris, France
cCorresponding author: Ali Chouaib, 315, 1 Boulevard Jourdan, 75014, Paris, France
Manuscript accepted for publication June 8, 2011
Short title: Spinal Cord Sarcoidosis and Neurogenic Bladder
doi: https://doi.org/10.4021/jnr21e
| Abstract | ▴Top |
We report a case of spinal cord sarcoidosis in which urodynamic studies showed neurogenic bladder dysfunction. A 56-year-old Caucasian woman developed progressive weakness of both lower extremities causing walking disturbance. Two months later, she became unable to walk, and she gradually developed urinary urgency, nocturnal urinary frequency, and urge urinary incontinence. Spinal MRI disclosed dorsal lesion, with atrophy of the cervical cord; the brain MRI was normal. Cerebrospinal fluid (CSF) analysis showed elevated proteins. Serum angiotensin-converting enzyme (ACE) level was moderately high. The tuberculin skin test was negative. The thoraco-abdomino-pelvien scanner showed a suspicious lesion in the liver. The draining biopsy of the liver revealed non-caseating epithelioid granuloma. This finding confirmed the diagnosis of spinal cord sarcoidosis. The urodynamic study showed detrusor hyperreflexia. Prednisolone treatment improved the urinary and neurological symptoms. The spinal lesion seems to be responsible for the mictional disturbance in our patient with spinal cord sarcoidosis.
Keywords: Sarcoidosis; Spinal cord; Urodynamics; Neurogenic bladder
| Introduction | ▴Top |
Sarcoidosis is a multisystem inflammatory granulomatous disease of unknown etiology. Neurosarcoidosis (NS), sarcoidosis involving the nervous system, is thought to be much rarer, occurring in less than 5% of patients with systemic sarcoidosis [1]. However, in a half of them, the presenting manifestation is neurologic without any evidence of systemic involvement, making early diagnosis and management difficult.
Sarcoidosis of the spinal cord is rare with an incidence estimated at 0.43% [2].
Mictional disturbance is occasionally described in patients with spinal cord sarcoidosis, but few urodynamic findings are available to our knowledge [3].
We describe a case history and the result of urodynamic study in a patient with spinal cord sarcoidosis.
| Case Report | ▴Top |
Case history
A 56-year-old Caucasian woman developed progressive weakness of both lower extremities causing walking disturbance; two months later, she became unable to walk. However, she gradually developed urinary urgency, nocturnal urinary frequency (more than five times a night), and urge urinary incontinence. Physical examination noted a spastic paraparesis, tetrapyramidal irritation and instability. Spinal MRI disclosed dorsal lesion which appeared as a low signal intensity on T1 and high signal intensity on T2 (Fig. 1), with atrophy of the cervical cord (Fig. 2). The brain MRI was normal. Cerebrospinal fluid (CSF) analysis showed elevated proteins (0.86 mg/L). Serum angiotensin-converting enzyme (ACE) level was moderately elevated. The tuberculin skin test was negative. The initial phosphocalcic balance assessment was normal but repetitive controls put in evidence and hypercalciuria (51.85 g/L) with a hypophosphaturia. The thoraco-abdomino-pelvien computed tomography scanner showed a suspicious lesion in the liver. The draining biopsy of the liver revealed non-caseating epithelioid granuloma. This finding confirmed the diagnosis of spinal cord sarcoidosis.
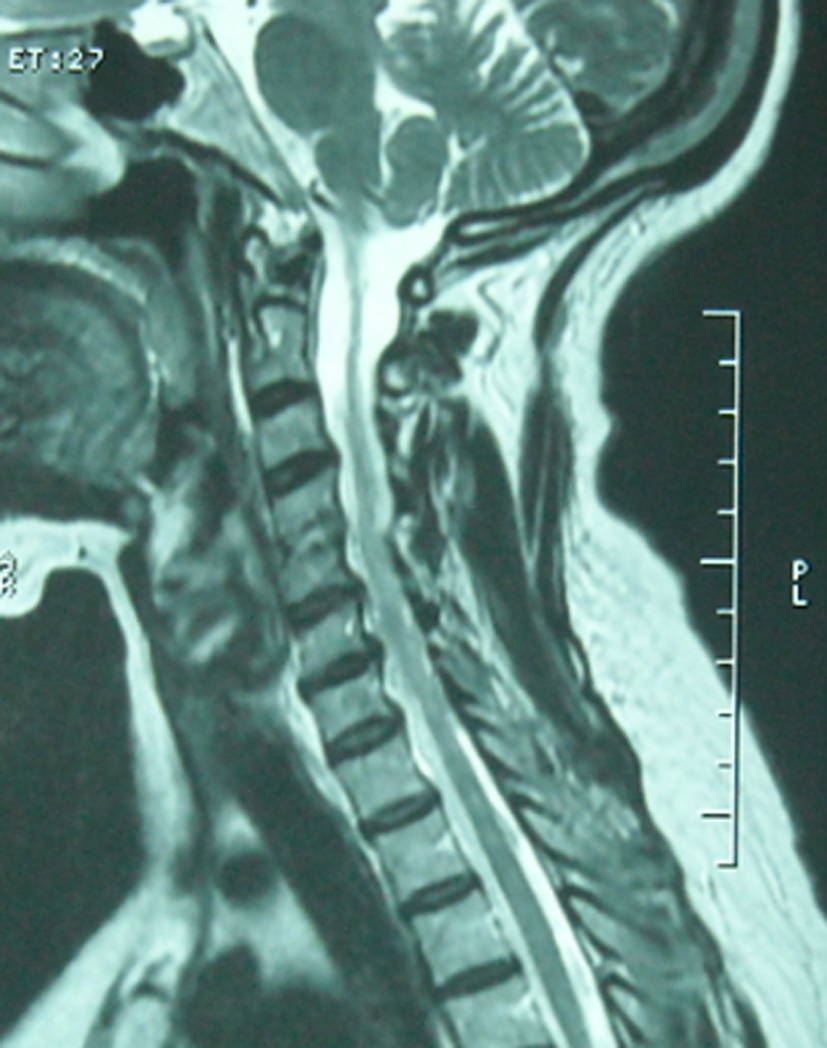 Click for large image | Figure 1. MRI of the spinal cord (sagittal plane), T2 weighted image. The T9 intramedullary region (dorsal spine) of the cord was high signal intensity. |
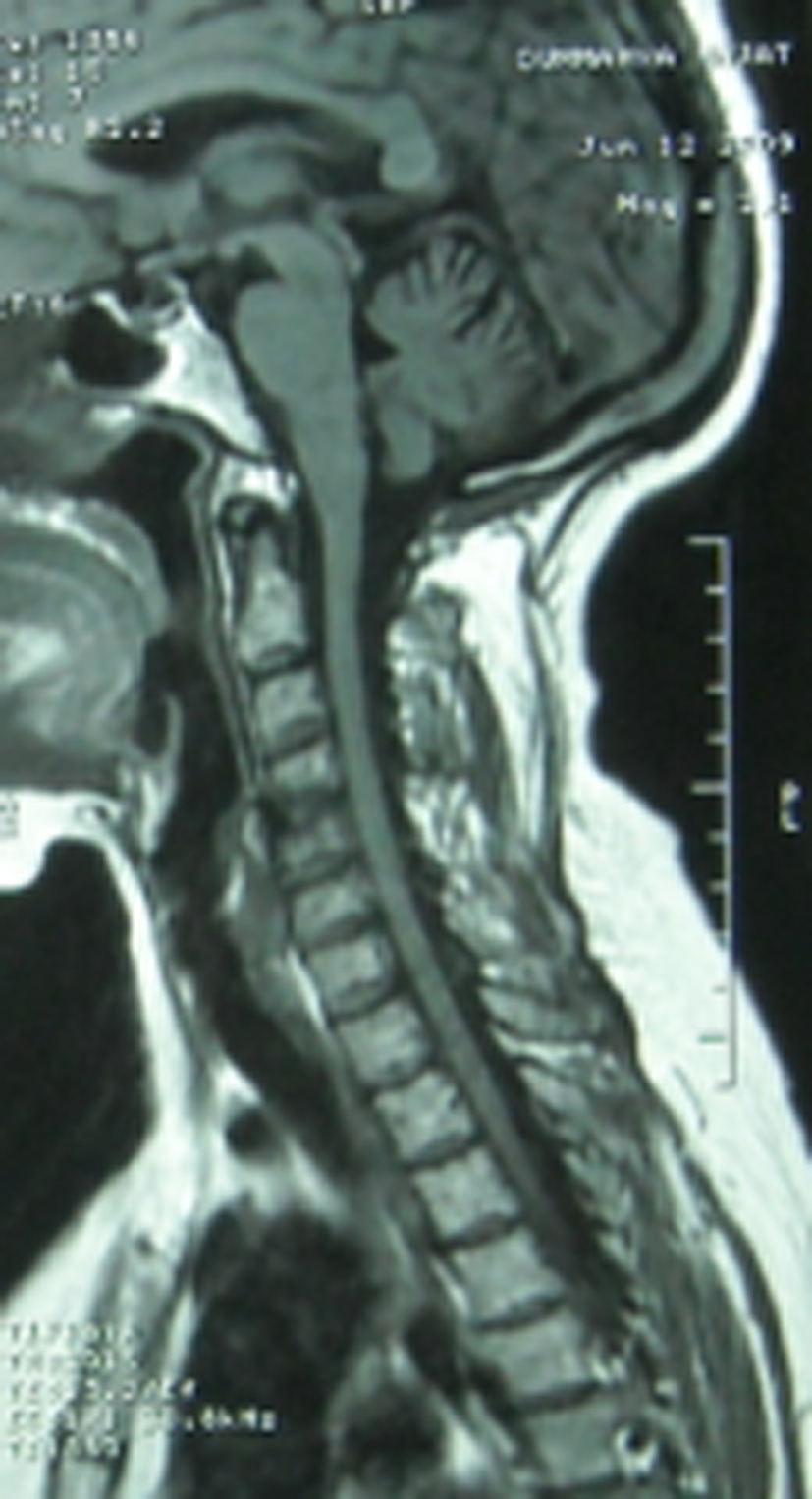 Click for large image | Figure 2. MRI of the spinal cord (sagittal plane), T1 weighted image. The T9 intramedullary region (dorsal spine) of the cord was low signal intensity, with atrophy of cervical cord. |
The patient underwent corticoid therapy (500 mg/day of intravenous methylprednisolone over 5 succeeding days) and started taking oral prednisolone (40 mg/day). After four weeks, a control MRI of the spine showed improvement. The patient continued to improve gradually and her urinary symptoms were ameliorated, and the treatment was tapered down by 10 mg every week to a maintenance dose of 10 mg/day. Walking became possible with two sticks.
Urodynamic study findings
Urodynamic study was done one month after the start of treatment. The urine culture was sterile and cystoscopy was normal. After voluntary voiding, we measured post-micturition residuals, and their normal volume is under 30 mL. After inserting a 12-F side-hole catheter, we measured urethral pressure profilometry with infusing 2 mL/min of sterile water. Normal range of maximum urethral closure pressure (UPmax) in our laboratory is > 41 cm H2O but < 82 cm H2O. After inserting an 8-F double-lumen transurethral catheter and a concentric needle electrode, medium-fill (50 mL/min) water cystometry with simultaneous sphincter EMG was done by a urodynamic computer (Lifetech; Janus) in a supine position. Normal range of first sensation is > 100 mL but < 300 mL, and bladder capacity is > 200 mL but < 600 mL. The methods and definitions used for the urodynamic studies conformed to the standards proposed by the International Continence Society [Abrams et al., 1989]. The patient had no amount of post-micturition residual. External sphincter EMG revealed exaggerated bulbocavernosus reflex, but no evidence of uninhibited sphincter relaxation or detrusor-sphincter dyssynergia. Water cystometry revealed decreased bladder volume at first sensation of 80 mL, bladder capacity of 230 mL, and a marked detrusor hyperreflexia (Fig. 3). The maximum urethral closure pressure was 60 cm H2O. Though we could not repeat urodynamic studies, the corticosteroid therapy has improved urinary symptoms.
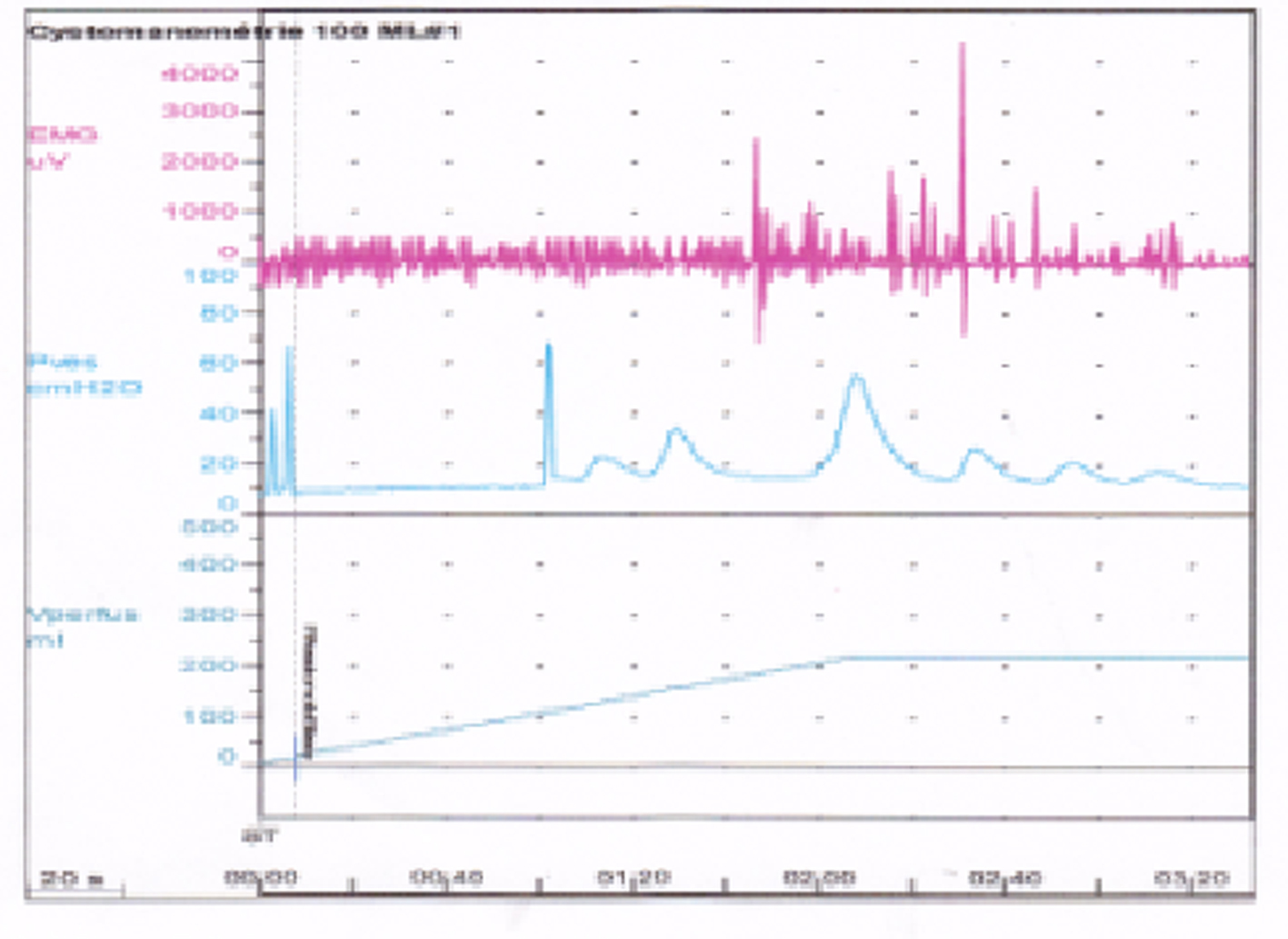 Click for large image | Figure 3. EMG-cystometry, involuntary detrusor contraction. |
| Discussion | ▴Top |
Sarcoidosis is a multisystem granulomatous disease of unknown etiology that most commonly affects the lungs, eyes and skin. Sarcoidosis affects the nervous system in 5% of patients [1], being considered a rare manifestation. Sarcoidosis of the spinal cord is rare with an incidence estimated at 0.43% [2]. Like other spinal cord injuries, the spinal cord sarcoidosis may be presented with paraparesis, quadriparesis, sensory changes, autonomic dysreflexia, or radicular symptoms [4, 5].
MRI is very sensitive in localizing the lesions; lesions enhance with gadolinium except late in the disease, when cord atrophy occurs. Radiologic aspects are not specific and highly variable [3, 6].
The diagnosis is suspected in patients with active systemic sarcoidosis; however, it is extremely difficult to make the diagnosis when spinal cord involvement is the first or sole manifestation of the disease. Biopsy of the spinal cord is an invasive procedure and is not without risk. The decision to obtain a biopsy of the spinal cord should be taken only after an extensive search for other organ involvement [3, 6].
This case is an example of fruitful search of other organ involvement and avoidance to biopsy the spinal cord.
For the treatment of spinal cord sarcoidosis, corticosteroids are the therapy of choice.
Urinary problems caused by neurosarcoidosis are exceptional, especially for spinal cord sarcoidosis. Detailed description is rare and few urodynamic findings are available on the mictional disturbance in spinal cord sarcoidosis. In most published cases, the authors reported only the clinical description of the lower urinary tract disorders associated with neurosarcoidosis. Fitzpatrick KJ et al described the first case of neurogenic lower urinary tract dysfunction associated with spinal cord sarcoidosis [7]. Urodynamic findings of detrusor hyperreflexia with detrusor-sphincter dyssynergia correlate with magnetic resonance imaging (MRI) examination which found intramedullary involvement at the mid-thoracic level.
Sakaibara R et al [8] reported a 42-year-old woman who began to have a slowly progressive spastic gait, left hand numbness, urinary urgency/frequency, and voiding difficulty which worsened gradually for a year. Two months later she became unable to walk without an aid. Spinal MRI disclosed C2-7 cord swelling. She also developed bilateral hilar lymphadenopathy, uveitis, and an increased serum concentration of angiotensin-converting enzyme (ACE). Endoscopic lymph node biopsy showed non-caseating epithelioid granuloma. These findings and the clinical features confirmed the diagnosis of spinal cord sarcoidosis.
Conclusion
Spinal cord sarcoidosis is a rare but well-documented condition; however in several cases the presenting manifestation is neurologic without any evidence of systemic involvement, making early diagnosis and management difficult. The spinal lesions may be mainly responsible for mictional disturbance in patients with spinal cord sarcoidosis.
The present case and the previous reports reflect the phenotypic variability of this disorder, and the benefit to perform urodynamic studies.
| References | ▴Top |
- Joseph FG, Scolding NJ. Sarcoidosis of the nervous system. Pract Neurol. 2007;7(4):234-244.
pubmed doi - Bogousslavsky J, Hungerbuhler JP, Regli F, Graf HJ. Subacute myelopathy as the presenting manifestation of sarcoidosis. Acta Neurochir (Wien). 1982;65(3-4):193-197.
pubmed doi - Saleh S, Saw C, Marzouk K, Sharma O. Sarcoidosis of the spinal cord: literature review and report of eight cases. J Natl Med Assoc. 2006;98(6):965-976.
pubmed - Hamasaki T, Noda M, Kamei N, Yamamoto S, Ochi M, Yasunaga Y. Intradural extramedullary mass formation in spinal cord sarcoidosis: case report and literature review. Spine (Phila Pa 1976). 2003;28(20):E420-423.
pubmed - Sakakibara R, Hattori T, Uchiyama T, Yamanishi T. Micturitional disturbance in a patient with neurosarcoidosis. Neurourol Urodyn. 2000;19(3):273-277.
pubmed doi - Fitzpatrick KJ, Chancellor MB, Rivas DA, Kumon H, Mandel S, Manon-Espaillat R. Urologic manifestation of spinal cord sarcoidosis. J Spinal Cord Med. 1996;19(3):201-203.
pubmed - Sakaibara R, Uchiyama T, Kuwabara S, Kawaguchi N, Nemoto I, Nakata M, Hattori H. Autonomic dysreflexia due to neurogenic bladder dysfunction; an unusual presentation of spinal cord sarcoidosis. J Neurol Neurosurg Psychiatry. 2001;71(6):819-820.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
