| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website http://www.neurores.org |
Case Report
Volume 4, Number 5-6, December 2014, pages 138-140
A Case of Infantile Metachromatic Leukodystrophy
Vaibhav S. Lokhandea, b, Anil Gaura
aDepartment of Physical Medicine and Rehabilitation, All India Institute of Physical Medicine and Rehabilitation, K Khadey Road, Haji Ali, Mumbai (W) 400 034, India
bCorresponding Author: Vaibhav S. Lokhande, Department of Physical Medicine and Rehabilitation, All India Institute of Physical Medicine and Rehabilitation, K Khadey Road, Haji Ali, Mumbai (W) 400 034, India
Manuscript accepted for publication August 12, 2014
Short title: Infantile Metachromatic Leukodystrophy
doi: http://dx.doi.org/10.14740/jnr294e
| Abstract | ▴Top |
Metachromatic leukodystrophy (MLD) is the neurometabolic disease caused by deficiency of enzyme arylsulfatase A resulting in deficiency of sulfatide degradation. The responsible gene is arylsulfatase A gene. We report a case of the infantile MLD that was confirmed by means of enzyme studies, nerve conduction velocity and typical MRI of brain findings.
Keywords: Infantile; Metachromatic leukodystrophy; Arylsulfatase A; ARSA gene; MRI brain
| Introduction | ▴Top |
Metachromatic leukodystrophy (MLD) is the typical white matter disease which belongs to the lysosomal sphingolipid storage group, and it is inherited in the autosomal recessive way [1]. MLD is caused by the deficiency of enzyme arylsulfatase A (ARSA) resulting in the deficiency of sulfatide degradation and the target gene is ARSA gene. The accumulation of sulfatide triggers leukodystrophy. The incidence of MLD is reported as about 1 per 100,000 live births in the European population, and is found at even lower rate in Asia [2, 3]. Clinically, it shows a wide range of spectrum with respect to the age of onset, the rate of progression and the initial following: 1) the late infantile form of disease that starts before the age of 2 or 3 years, 2) the juvenile form that starts between 2 or 3 and 16 years, and 3) the adult form that presents its first symptoms after the age of 16 years [4-6].
| Case Report | ▴Top |
A 2 years and 6 months old male patient came with chief complaints of developmental delay and generalized tightness which started developing at the age of 1 year, and inability to seat and stand. He had no specific birth history and showed normal pattern of development including independent walking before the onset of symptoms. The developmental regression progressed continuously. His family history was found to be negative. Parents noticed weakness in bilateral lower limb and he was taken to general physician, where he was investigated. Routine investigations were found to be normal except serum calcium level was low. Hence he was treated with calcuim and vitamin-D supplements. Parents noticed no improvement. On clinical examination bilateral knee reflex exaggerated and Babinski’s sign was positive. So MRI of brain was done which was suggestive of T2 hyperintense signals in bilateral fronto-parietal, parieto-occipital white matter, corona radiata and posterior capsule. This was likely suggestive of dysmylination/demylination sequalae to MLD (Fig. 1-3).
 Figure 1. MRI of brain showing T2 hyperintense signals in bilateral fronto-parietal, parieto-occipital white matter. Figure 1. MRI of brain showing T2 hyperintense signals in bilateral fronto-parietal, parieto-occipital white matter. |
 Figure 2. MRI of brain showing T2 hyperintense signals in posterior capsule. Figure 2. MRI of brain showing T2 hyperintense signals in posterior capsule. |
 Figure 3. MRI of brain showing T2 hyperintense signals in corona radiata. Figure 3. MRI of brain showing T2 hyperintense signals in corona radiata. |
Nerve conduction velocity study was done for lower limbs weakness which was indicative of bilateral sensory motor neuropathy.
Arylsulfatase A enzyme activity in leukocytes was tested and found to be decreased to 5.3% of normal control value. Thus, the patient was confirmed to have metachromatic leukodystrophy (method: artificial chromogenic and flurogenic substrates (Fig. 4)).
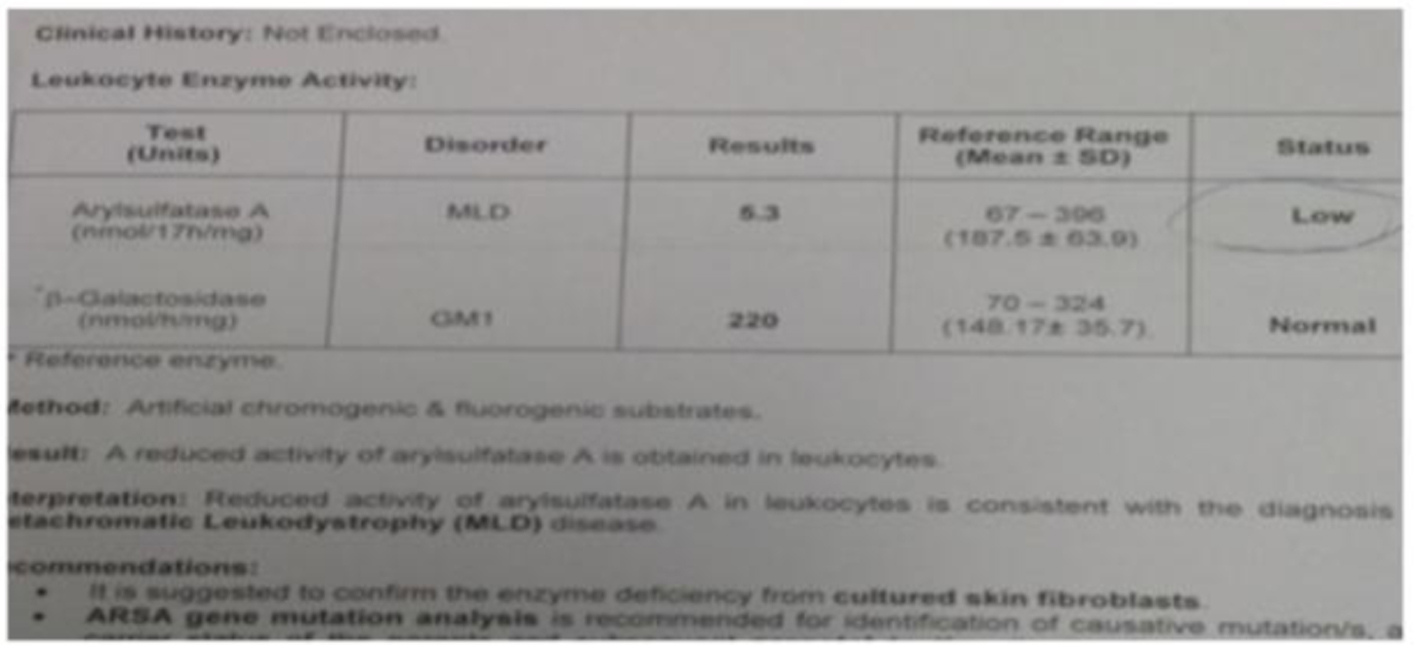 Figure 4. Arylsulfatase A enzyme activity in leukocytes by “artificial chromogenic and flurogenic substrates” method. Figure 4. Arylsulfatase A enzyme activity in leukocytes by “artificial chromogenic and flurogenic substrates” method. |
| Discussion | ▴Top |
MLD is a lysosomal storage disease from the family of leukodystrophies and among the sphingolipidoses it affects the metabolism of sphingolipids. Leukodystrophies affect the growth and/or development of myelin, the fatty covering which acts as an insulator around nerve fibers throughout the central and peripheral nervous systems. MLD involves cerebroside sulfate accumulation. MLD has an autosomal recessive inheritance pattern [7].
There is currently no treatment or cure for MLD and future treatment options are currently being investigated. These include gene therapy, enzyme replacement therapy, substrate reduction therapy and potentially enzyme enhancement therapy.
Our patient is not able to sit, therefore seating device was provided from our institute (Fig. 5). For bilateral lower limb spasticity “knee ankle foot orthosis” was provided. Prognosis was explained and also medical and social counselling was done to parents. We were not able to do ARSA gene testing due to lack of affordability.
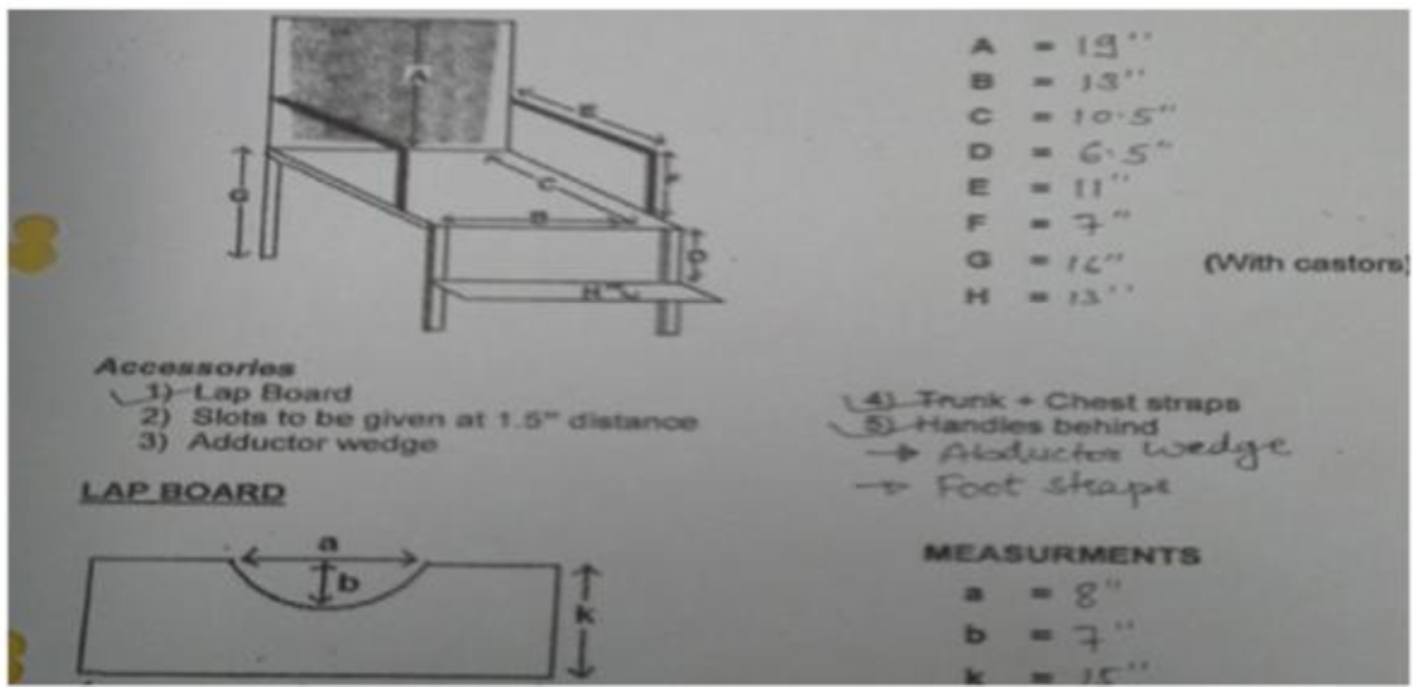 Figure 5. Seating device for patient designed by our institute. Figure 5. Seating device for patient designed by our institute. |
| References | ▴Top |
- Sandhoff R, Hepbildikler ST, Jennemann R, Geyer R, Gieselmann V, Proia RL, Wiegandt H, et al. Kidney sulfatides in mouse models of inherited glycosphingolipid disorders: determination by nano-electrospray ionization tandem mass spectrometry. J Biol Chem. 2002;277(23):20386-20398.
doi pubmed - Heim P, Claussen M, Hoffmann B, Conzelmann E, Gartner J, Harzer K, Hunneman DH, et al. Leukodystrophy incidence in Germany. Am J Med Genet. 1997;71(4):475-478.
doi - Poorthuis BJ, Wevers RA, Kleijer WJ, Groener JE, de Jong JG, van Weely S, Niezen-Koning KE, et al. The frequency of lysosomal storage diseases in The Netherlands. Hum Genet. 1999;105(1-2):151-156.
doi pubmed - Biffi A, Cesani M, Fumagalli F, Del Carro U, Baldoli C, Canale S, Gerevini S, et al. Metachromatic leukodystrophy - mutation analysis provides further evidence of genotype-phenotype correlation. Clin Genet. 2008;74(4):349-357.
doi pubmed - MacFaul R, Cavanagh N, Lake BD, Stephens R, Whitfield AE. Metachromatic leucodystrophy: review of 38 cases. Arch Dis Child. 1982;57(3):168-175.
doi pubmed - Lugowska A, Amaral O, Berger J, Berna L, Bosshard NU, Chabas A, Fensom A, et al. Mutations c.459+1G>A and p.P426L in the ARSA gene: prevalence in metachromatic leukodystrophy patients from European countries. Mol Genet Metab. 2005;86(3):353-359.
doi pubmed - Le Tao, Bhushan Vikas, Hofmann Jeffrey. First Aid for the USMLE Step 1. McGraw-Hill. 2012:117.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
