| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website http://www.neurores.org |
Case Report
Volume 5, Number 6, December 2015, pages 294-295
The Hazards of Recreational Drug Use: A Case of Toxic Leukoencephalopathy
Clianna Lavellea, b, Muhammad Fahmi Ismaila
aSouth Lee Mental Health Service, Cork University Hospital, Wilton, Cork, Ireland
bCorresponding Author: Clianna Lavelle, Acute Mental Health Unit, Cork University Hospital, Wilton, Cork, Ireland
Manuscript accepted for publication October 30, 2015
Short title: Toxic Leukoencephalopathy
doi: http://dx.doi.org/10.14740/jnr362e
| Abstract | ▴Top |
Toxic leukoencephalopathy is a disorder characterized by the alteration of myelin in white matter tracts secondary to exposure to neurotoxic substances. This case describes the neuropsychiatric presentation of toxic leukoencephalopathy. Brain imaging confirms a diagnosis of toxic leukoencephalopathy secondary to polysubstance overdose. The patient made a significant recovery following admission to hospital.
Keywords: Hazard; Recreational drug; Toxic leukoencephalopathy
| Introduction | ▴Top |
Toxic leukoencephalopathy is a disorder characterized by the alteration of myelin in white matter tracts secondary to exposure to neurotoxic substances [1]. Its clinical presentation may vary from inattention and personality changes to coma and death [1]. Advances in magnetic resonance imaging (MRI) have contributed significantly to its diagnosis in patients presenting with neuropsychiatric symptoms in the setting of recent toxin exposure [1].
| Case Report | ▴Top |
We report a case of a 45-year-old single man with a background history of depression, alcohol dependence and polysubstance abuse who presented on referral from his general practitioner to an acute psychiatric facility with a 2-week history of confusion, memory difficulties and bizarre, disorganized behavior in the context of a recent unintentional overdose of heroin and amphetamines for which he had been briefly hospitalized three weeks previously.
At the time of his admission to the general hospital following the overdose, he was found to have a GCS of 9 with pinpoint pupils and a marked left-sided upper limb weakness. His medical issues at that time included rhabdomyolysis, acute kidney injury, transaminitis and a left radial neuropathy. He was treated with intravenous naloxone and thiamine and other supportive measures before being discharged home with a view to neurological and psychological follow-up.
Shortly after his discharge, however, he suffered a dramatic decline in cognition resulting in bizarre, erratic behaviors which were quite out of keeping with his character. For example, he would put socks on over his shoes and once had entered a jewellery store in search of pet food. He had also tried to exit a moving vehicle. He expressed fears that he was becoming “autistic” and reported thought insertion along with suicidal ideation. He was admitted under psychiatry for observation of his mental state.
On examination, he was noted to be anxious, disoriented, easily startled and distracted, and globally cognitively impaired. He demonstrated left-right disorientation and was unable to follow simple commands. MOCA testing revealed a score of 3/30. Laboratory parameters were within normal ranges. Initial CT of brain during first admission revealed subtle bilateral low attenuation changes in the pallidum. Follow-up MRI of brain on admission to the psychiatric unit showed extensive confluent deep and subcortical white matter signal changes consistent with a diagnosis of toxic leukoencephalopathy secondary to polysubstance overdose (Fig. 1). EEG demonstrated diffuse slow wave activity consistent with encephalopathy. Neuropsychological testing showed that his cognitive functioning was in the extremely low range consistent with a mild-moderate intellectual disability.
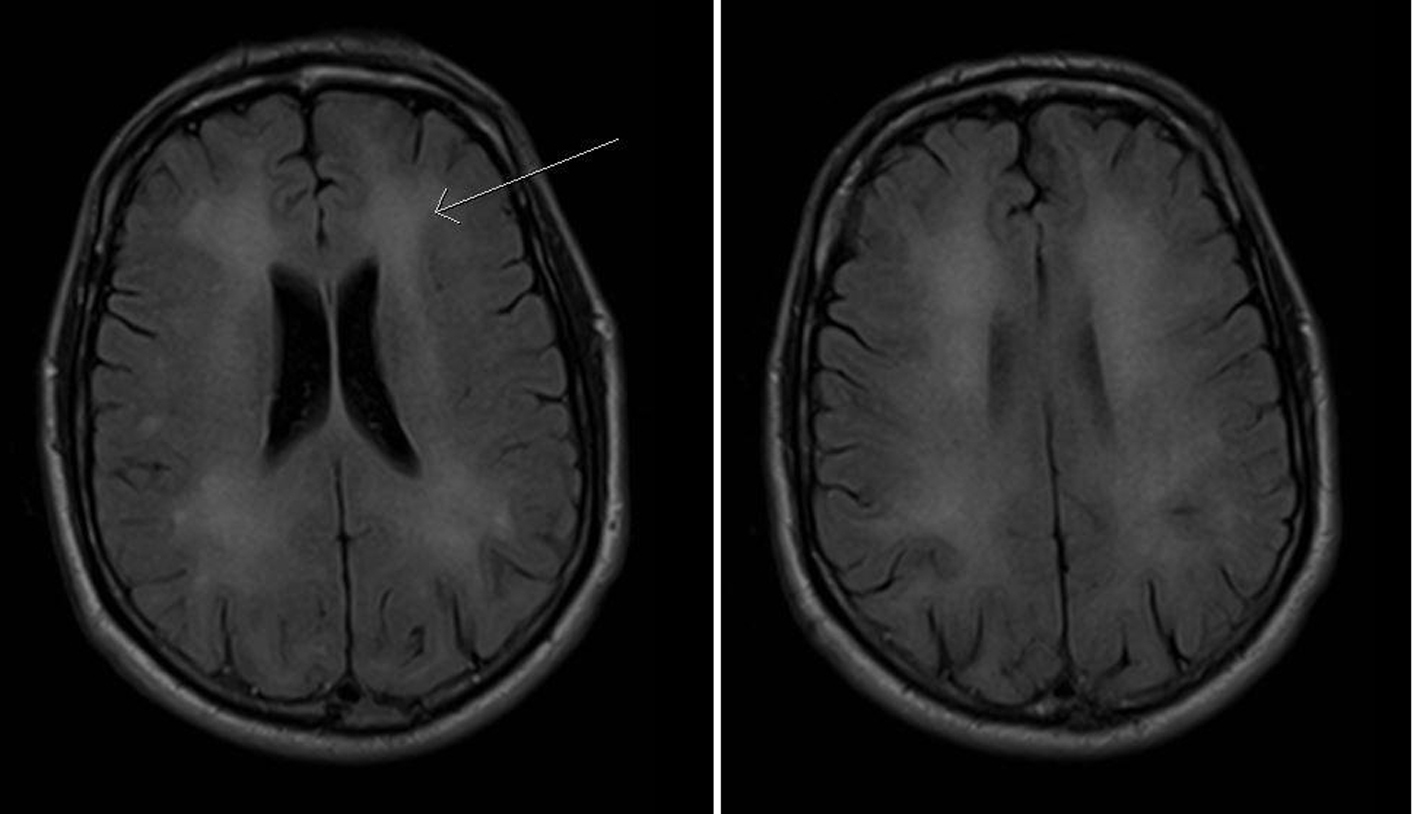 Click for large image | Figure 1. Axial T2-weighted MRI brain images showing extensive confluent symmetrical white matter hyperintensities in both cerebral hemispheres (arrow). These demonstrate extensive injury to cerebral white matter in keeping with a toxic leukoencephalopathy. |
An extensive multidisciplinary programme was put in place for the patient who included our colleagues in neurology, speech and language therapy, occupational therapy, physiotherapy and psychology. The patient’s recovery was slow but steady, with significant improvements noted in his cognitive ability and his overall level of functioning. He was subsequently transferred to a rehabilitation facility where his progress continued.
| Discussion | ▴Top |
Toxic leukoencephalopathy was first reported in 1982 and has been associated with exposure to a range of toxins including therapeutic drugs and illicit substances such as heroin and cocaine [2-4]. It principally affects white matter tracts, resulting in a spectrum of clinical features ranging from inattention and disorientation to dementia and death [1]. Its pathophysiology, albeit unclear, is thought to involve a hypoxic-ischemic injury to the white matter of the cerebrum which results in widespread, confluent vacuolation of the latter, known as spongiform degeneration or leukoencephalopathy [5]. Neuroradiologic abnormalities are best seen in T2-weighted MRI brain scans which typically reveal bihemispheric white matter abnormalities [4]. Clinical outcomes can range from full recovery in some, over a 3- to 12-month period, to rapidly fatal in others [3, 6].
Toxic leukoencephalopathy should be considered as part of the differential diagnosis in any case of new-onset neurobehavioral changes following exposure to toxins such as heroin, amphetamines or other drugs of abuse. Special attention should be drawn to the possibility of a delayed-onset presentation, often with psychiatric symptoms, and to the crucial role of the multidisciplinary team in enabling a progressive, steady recovery. Anticipation and early recognition of toxic leukoencephalopathy are crucial in preventing its potentially severe complications and in enabling recovery in patients known to have engaged in recreational drug misuse.
Grant Support
None.
Conflict of Interest
None.
| References | ▴Top |
- Filley CM, Kleinschmidt-DeMasters BK. Toxic leukoencephalopathy. N Engl J Med. 2001;345(6):425-432.
doi pubmed - Wolters EC, van Wijngaarden GK, Stam FC, Rengelink H, Lousberg RJ, Schipper ME, Verbeeten B. Leucoencephalopathy after inhaling "heroin" pyrolysate. Lancet. 1982;2(8310):1233-1237.
doi - Maschke M, Fehlings T, Kastrup O, Wilhelm HW, Leonhardt G. Toxic leukoencephalopathy after intravenous consumption of heroin and cocaine with unexpected clinical recovery. J Neurol. 1999;246(9):850-851.
doi pubmed - Ryan A, Molloy FM, Farrell MA, Hutchinson M. Fatal toxic leukoencephalopathy: clinical, radiological, and necropsy findings in two patients. J Neurol Neurosurg Psychiatry. 2005;76(7):1014-1016.
doi pubmed - Blasel S, Hattingen E, Adelmann M, Nichtweiss M, Zanella F, Weidauer S. Toxic leukoencephalopathy after heroin abuse without heroin vapor inhalation: MR imaging and clinical features in three patients. Clin Neuroradiol. 2010;20(1):48-53.
doi - Shprecher D, Mehta L. The syndrome of delayed post-hypoxic leukoencephalopathy. NeuroRehabilitation. 2010;26(1):65-72.
pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
