| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website http://www.neurores.org |
Case Report
Volume 6, Number 5-6, December 2016, pages 106-110
Posterior Reversible Encephalopathy Syndrome: Case Report
Mahesh Babu Sodalaguntaa, Sreenivasa Rao Sudulaguntab, g, Monica Kumbhatc, Mona Sepehrard, Aravinda Settikere Natarajue, Shiva Kumar Bangalore Rajaf
aK. S. Hegde Medical College, Mangalore, India
bColumbia Asia Hospital, Kirloskar Business Park, Hebbal, Bangalore, India
cSri Ramachandra Medical College, No. 1, Ramachandra Nagar, Porur, Chennai, Tamil Nadu 600116, India
dBaptist Hospital, Bangalore, India
eColumbia Asia Hospital, Hebbal, Bangalore, India
fDepartment of General Medicine, Dr. B. R. Ambedkar Medical College, Bangalore, India
gCorresponding Author: Sreenivasa Rao Sudulagunta, Columbia Asia Hospital, Kirloskar Business Park, Hebbal, Bangalore 560024, India
Manuscript accepted for publication November 23, 2016
Short title: Posterior Reversible Encephalopathy Syndrome
doi: https://doi.org/10.14740/jnr402w
| Abstract | ▴Top |
Posterior reversible encephalopathy syndrome (PRES) is a clinico-radiological syndrome characterized by headache, seizures, altered mental status, and visual loss, as well as white matter vasogenic edema affecting the posterior occipital and parietal lobes of the brain predominantly. This clinical syndrome is increasingly recognized due to improvement and availability of brain imaging, specifically magnetic resonance imaging (MRI). A 35-year-old female with history of unsafe abortion and massive blood transfusion 10 days ago was brought to the emergency room with three episodes of generalized tonic clonic seizures, urinary incontinence and altered sensorium since 3 hours. Brain MRI showed bilateral occipital, parietal, frontal cortex and subcortical white matter T2/fluid-attenuated inversion recovery (FLAIR) hyperintensities, suggestive of PRES. Patient improved after management with intravenous fluids, antibiotics, antiepileptics and monitoring of blood pressure. If recognized and treated early, the clinical syndrome commonly resolves within a week. PRES can be a major problem in rapid and massive blood transfusion. High index of suspicion and prompt treatment can reduce morbidity and mortality, and pave the path for early recovery.
Keywords: Posterior reversible encephalopathy syndrome; Blood transfusion; Brain MRI; Antiepileptics
| Introduction | ▴Top |
Posterior reversible encephalopathy syndrome (PRES) is a clinico-radiological syndrome characterized by symptoms including headache, seizures, altered consciousness, and visual disturbances [1, 2]. PRES was first described in 1996 by Hinchey et al [3]. Shortly after the description in 1996, two other case series were published [4, 5]. This condition has been known by various names previously (reversible posterior leukoencephalopathy syndrome, reversible posterior cerebral edema syndrome, and reversible occipital parietal encephalopathy). PRES is now the widely accepted term [6, 7]. It is commonly but not always associated with acute hypertension [1, 2]. This clinical syndrome is increasingly recognized, commonly because of improvement and availability of brain imaging.
The major clinical conditions associated with PRES are represented in Table 1 [6]. There is wide variation in the severity of clinical symptoms, i.e., the visual disturbance can vary from blurred vision, homonymous hemianopsia to cortical blindness. Altered consciousness may vary from mild confusion or agitation, to coma. Other symptoms include nausea, vomiting and brainstem deficits. Seizures and status epilepticus are common, while non-convulsive status epilepticus may be more common than generalized status epilepticus [8].
 Click to view | Table 1. PRES-Associated Clinical Conditions [6, 8] |
Non-convulsive status should be cautiously observed in patients with prolonged altered consciousness, which may be mistaken commonly for postictal confusion. Signs include stereotypic movements like staring, head turning or eye blinking. Postictal confusion usually lasts for hours, but PRES and non-convulsive status can last for many days and can be mistaken for drug intoxication, psychosis or psychogenic states [9]. If recognized and treated early, the clinical syndrome commonly resolves within a week.
| Case Report | ▴Top |
A 35-year-old female was brought to the emergency room with history of three episodes of generalized tonic clonic seizures, urinary incontinence and altered sensorium since 3 h. Patient was referred from a local hospital for further management. Patient had headache prior to the onset of seizures. Patient relatives revealed that patient had unsafe abortion 10 days ago and later developed severe fatigue, shortness of breath and pedal edema. Husband expired 3 years ago due to unknown chronic illness. Due to severe anemia (hemoglobin: 3.4 g/dL) and ongoing blood loss, patient was transfused 5 units of blood in a local hospital. No history of hypertension was found as per medical records. No other significant history was available. On examination, vital signs of patient were normal. Patient was drowsy, not obeying commands, but withdrew limbs to painful stimuli, deep tendon reflexes were sluggish and a withdrawal response was seen in plantar reflex. There were no signs of meningeal irritation.
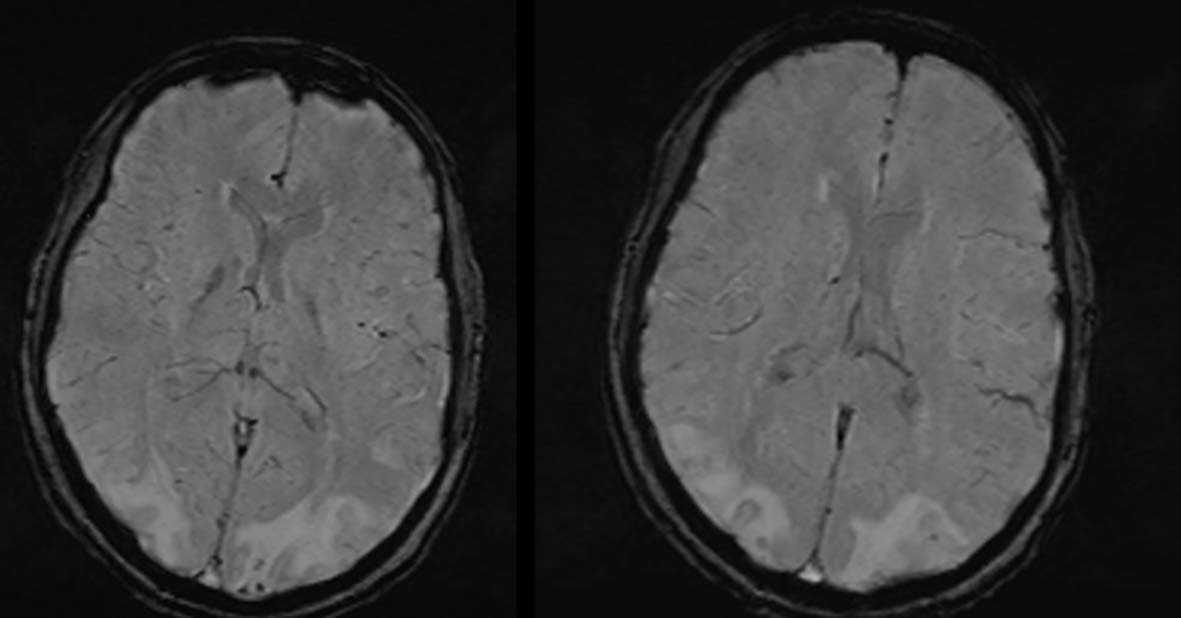
Laboratory examination revealed normal hemoglobin (13.8 g/dL), neutrophilic leukocytosis (18,000/dL), urinary tract infection (10 - 15 pus cells/hpf) and elevated C-reactive protein (4.7 mg/dL). Erythrocyte sedimentation rate, liver function tests and renal function tests were normal. Peripheral smear showed dimorphic anemia. Other blood tests, coagulation profile, autoantibodies, and neoplastic markers were normal. Cerebrospinal fluid analysis revealed an increase in protein level (50 mg/dL). Chest radiography and arterial blood gas analysis were normal. Brain magnetic resonance imaging (MRI) showed bilateral occipital, parietal, frontal cortex and subcortical white matter T2/fluid-attenuated inversion recovery (FLAIR) hyperintensities (Figs. 1-5), suggestive of PRES. Electroencephalography (EEG) showed bilateral temporal-occipital epileptiform discharges at times becoming general. Electrocardiography (ECG) showed incomplete right bundle branch block.
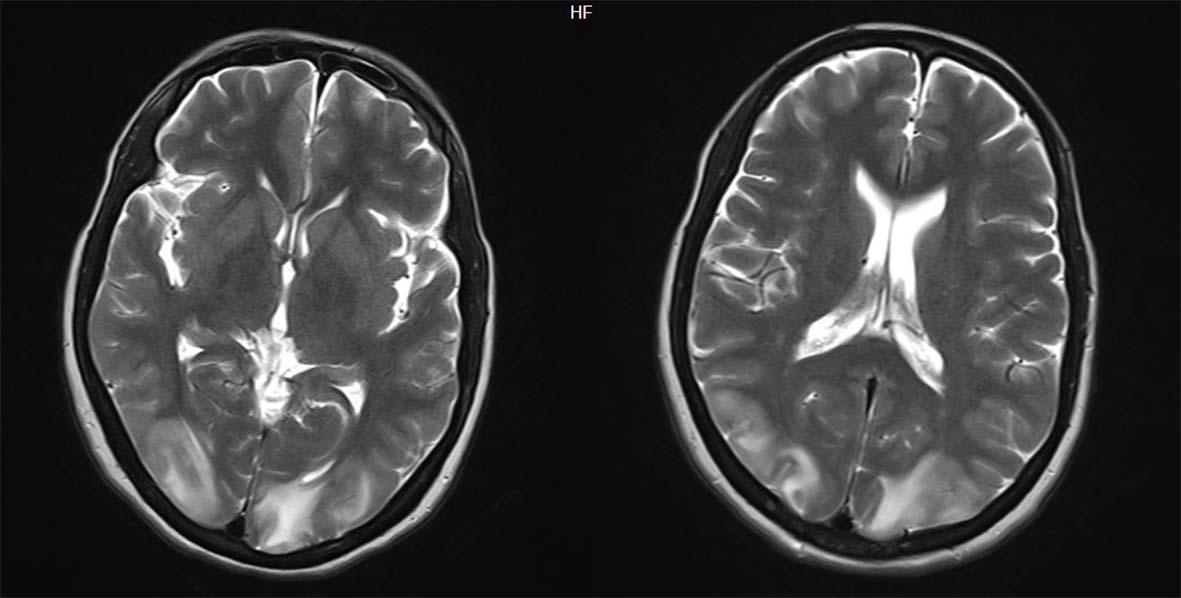 Click for large image | Figure 1. Axial view of magnetic resonance imaging of brain showing bilateral occipital, parietal, frontal cortex and subcortical white matter hyperintensities. |
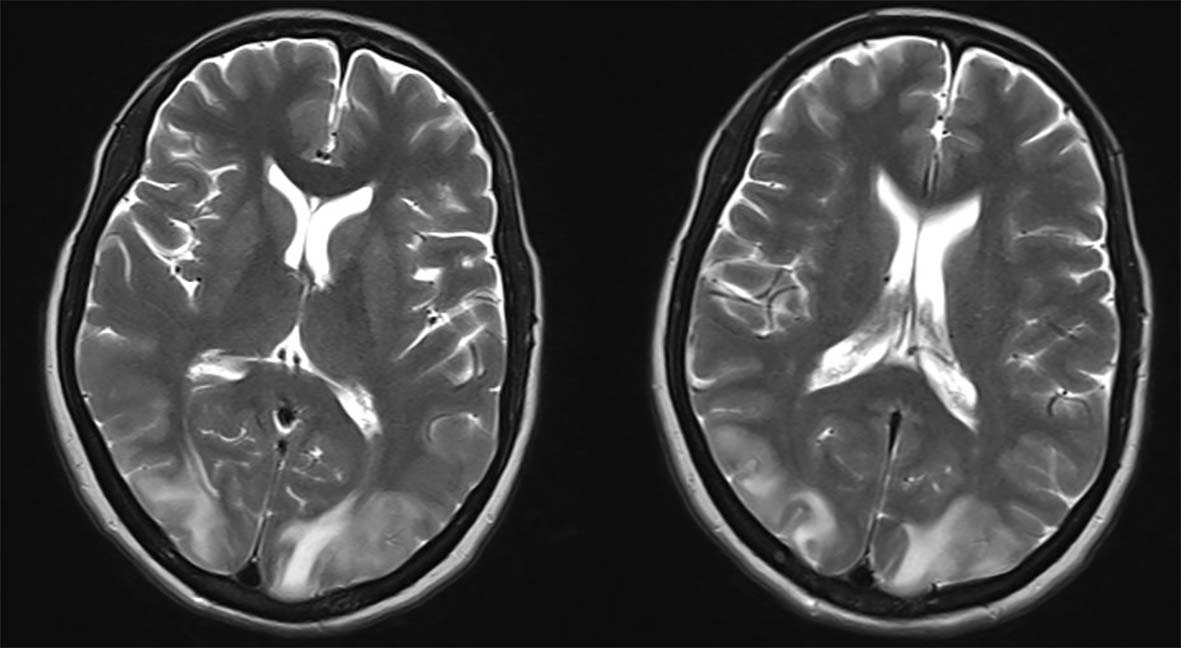 Click for large image | Figure 2. Axial view showing bilateral occipital, parietal, frontal cortex and subcortical white matter T2/FLAIR hyperintensities. |
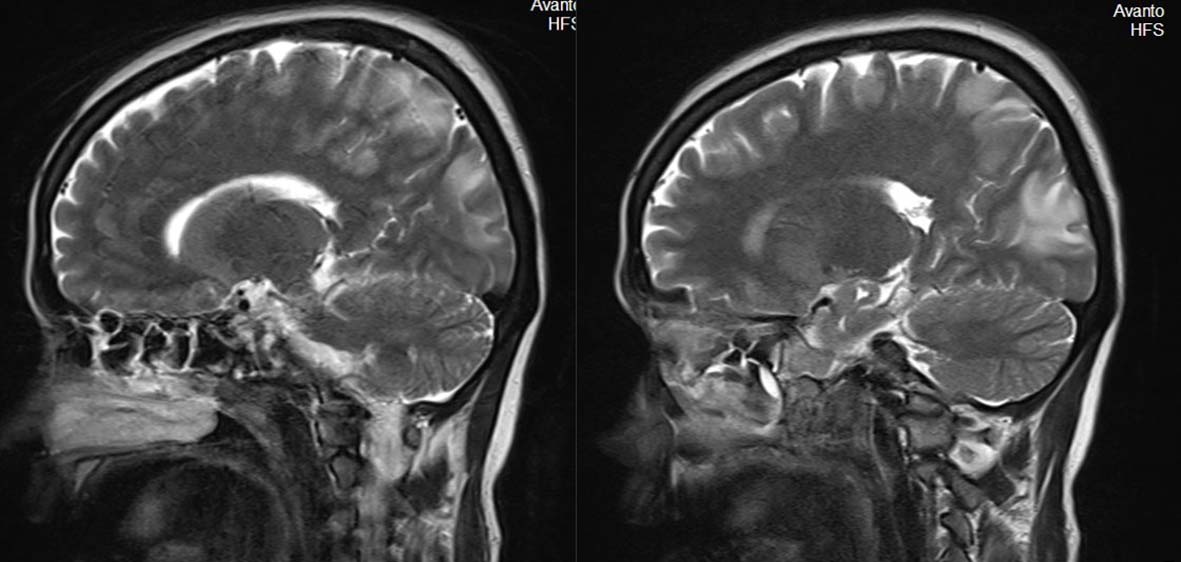 Click for large image | Figure 3. Sagittal view of magnetic resonance imaging of brain showing bilateral occipital, parietal, frontal cortex and subcortical white matter hyperintensities. |
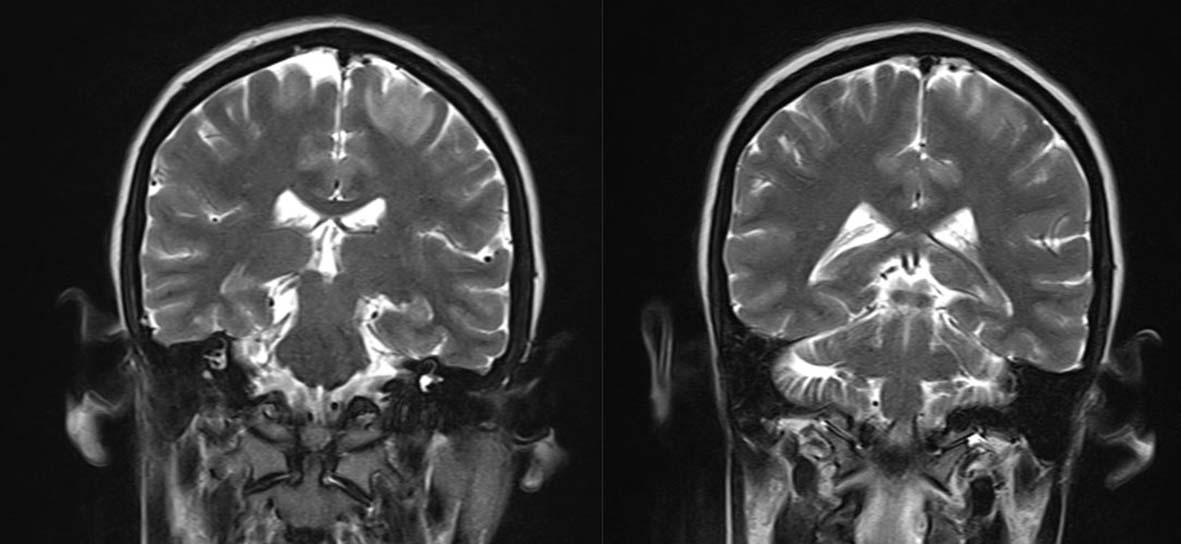 Click for large image | Figure 4. Coronal view of magnetic resonance imaging of brain showing bilateral occipital, parietal, frontal cortex and subcortical white matter hyperintensities. |
 Click for large image | Figure 5. Magnetic resonance imaging of brain showing bilateral occipital, parietal, frontal cortex and subcortical white matter T2/FLAIR hyperintensities. |
Patient was admitted in intensive care unit and was managed with intravenous fluids, antibiotics, antiepileptics and monitoring of blood pressure. Patient improved symptomatically in form of normal sensorium, leukocyte counts and vital signs. Patient was discharged after 7 days of admission at request. Follow-up after 1 week was uneventful.
| Discussion | ▴Top |
The term PRES has been used based on the similarity in appearance on imaging, the common location of the parietal-occipital lobe or “posterior” location of the lesions [10, 11]. The exact pathophysiological mechanism of PRES is still unclear [12]. Three hypotheses have been proposed till now, which include 1) cerebral vasoconstriction causing subsequent infarcts in the brain, 2) failure of cerebral auto-regulation with vasogenic edema, and 3) endothelial damage with blood-brain barrier disruption further leading to fluid and protein transudation in the brain [12-14]. The distinct imaging patterns in PRES are represented in Table 2 [15]. The reversible nature of PRES has been challenged recently based on new reports of permanent neurological impairment and mortality reaching 15% [16, 17].
 Click to view | Table 2. Imaging Patterns in PRES [15] |
No clinical studies are available till now regarding patients with PRES needing life-sustaining treatments. The improved knowledge and research about factors influencing the outcome of PRES will result in better early management, less morbidity and mortality. According to studies, delayed diagnosis and treatment may lead to mortality or irreversible neurological deficit [18, 19]. In hypertension-associated or drug-induced PRES, the effective therapy includes withdrawal of offending agent, immediate control of blood pressure, anti-convulsive therapy and temporary renal replacement therapy (hemodialysis/peritoneal dialysis) if required. In systemic lupus erythematosus (SLE)-related PRES, aggressive treatment with corticosteroids and cyclophosphamide is effective. Corticosteroids may improve vasogenic edema, but there is no solid evidence for usage in PRES.
Blood transfusion may cause a rapid increase in total blood volume, which further leads to cerebral blood flow overload. The case reports of PRES associated with blood transfusion are represented in Table 3 [20-26]. Abrupt or acute cerebral hyper-perfusion exceeding the capacity of auto-regulation of cerebral capillary perfusion pressure might result in vasogenic edema found in PRES. The possibility of severe anemia as the predisposing factor, due to inadequate supply of oxygen to the brain may result in dysfunction of endothelial cells, further causing a functional loss or damage to the integrity of the blood-brain barrier in capillary circulation which cannot be ruled out [26]. Our patient had no hypertension even transiently during the whole episode. In conclusion, PRES can be a major problem in rapid and massive blood transfusion. High index of suspicion and prompt treatment can reduce morbidity and mortality, and pave the path for early recovery.
 Click to view | Table 3. Case Reports of PRES Associated With Blood Transfusion |
Abbreviations
PRES: posterior reversible encephalopathy syndrome; SLE: systemic lupus erythematosus; FLAIR: fluid-attenuated inversion recovery
| References | ▴Top |
- McKinney AM, Short J, Truwit CL, McKinney ZJ, Kozak OS, SantaCruz KS, Teksam M. Posterior reversible encephalopathy syndrome: incidence of atypical regions of involvement and imaging findings. AJR Am J Roentgenol. 2007;189(4):904-912.
doi pubmed - Roth C, Ferbert A. The posterior reversible encephalopathy syndrome: what's certain, what's new? Pract Neurol. 2011;11(3):136-144.
doi pubmed - Hinchey J, Chaves C, Appignani B, Breen J, Pao L, Wang A, Pessin MS, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334(8):494-500.
doi pubmed - Schwartz RB, Jones KM, Kalina P, Bajakian RL, Mantello MT, Garada B, Holman BL. Hypertensive encephalopathy: findings on CT, MR imaging, and SPECT imaging in 14 cases. AJR Am J Roentgenol. 1992;159(2):379-383.
doi pubmed - Schwartz RB, Bravo SM, Klufas RA, Hsu L, Barnes PD, Robson CD, Antin JH. Cyclosporine neurotoxicity and its relationship to hypertensive encephalopathy: CT and MR findings in 16 cases. AJR Am J Roentgenol. 1995;165(3):627-631.
doi pubmed - Bartynski WS. Posterior reversible encephalopathy syndrome, part 1: fundamental imaging and clinical features. AJNR Am J Neuroradiol. 2008;29(6):1036-1042.
doi pubmed - Bartynski WS. Posterior reversible encephalopathy syndrome, part 2: controversies surrounding pathophysiology of vasogenic edema. AJNR Am J Neuroradiol. 2008;29(6):1043-1049.
doi pubmed - Hobson EV, Craven I, Blank SC. Posterior reversible encephalopathy syndrome: a truly treatable neurologic illness. Perit Dial Int. 2012;32(6):590-594.
doi pubmed - Kaplan PW. No, some types of nonconvulsive status epilepticus cause little permanent neurologic sequelae (or: "the cure may be worse than the disease"). Neurophysiol Clin. 2000;30(6):377-382.
doi - Provenzale JM, Petrella JR, Cruz LC, Jr., Wong JC, Engelter S, Barboriak DP. Quantitative assessment of diffusion abnormalities in posterior reversible encephalopathy syndrome. AJNR Am J Neuroradiol. 2001;22(8):1455-1461.
pubmed - Covarrubias DJ, Luetmer PH, Campeau NG. Posterior reversible encephalopathy syndrome: prognostic utility of quantitative diffusion-weighted MR images. AJNR Am J Neuroradiol. 2002;23(6):1038-1048.
pubmed - Vaughan CJ, Delanty N. Hypertensive emergencies. Lancet. 2000;356(9227):411-417.
doi - Shin KC, Choi HJ, Bae YD, Lee JC, Lee EB, Song YW. Reversible posterior leukoencephalopathy syndrome in systemic lupus erythematosus with thrombocytopenia treated with cyclosporine. J Clin Rheumatol. 2005;11(3):164-166.
doi pubmed - Min L, Zwerling J, Ocava LC, Chen IH, Putterman C. Reversible posterior leukoencephalopathy in connective tissue diseases. Semin Arthritis Rheum. 2006;35(6):388-395.
doi pubmed - Bartynski WS, Boardman JF. Distinct imaging patterns and lesion distribution in posterior reversible encephalopathy syndrome. AJNR Am J Neuroradiol. 2007;28(7):1320-1327.
doi pubmed - Burnett MM, Hess CP, Roberts JP, Bass NM, Douglas VC, Josephson SA. Presentation of reversible posterior leukoencephalopathy syndrome in patients on calcineurin inhibitors. Clin Neurol Neurosurg. 2010;112(10):886-891.
doi pubmed - Lee VH, Wijdicks EF, Manno EM, Rabinstein AA. Clinical spectrum of reversible posterior leukoencephalopathy syndrome. Arch Neurol. 2008;65(2):205-210.
doi pubmed - Kwon S, Koo J, Lee S. Clinical spectrum of reversible posterior leukoencephalopathy syndrome. Pediatr Neurol. 2001;24(5):361-364.
doi - Antunes NL, Small TN, George D, Boulad F, Lis E. Posterior leukoencephalopathy syndrome may not be reversible. Pediatr Neurol. 1999;20(3):241-243.
doi - Ito Y, Niwa H, Iida T, Nagamatsu M, Yasuda T, Yanagi T, Sobue G. Post-transfusion reversible posterior leukoencephalopathy syndrome with cerebral vasoconstriction. Neurology. 1997;49(4):1174-1175.
doi pubmed - Boughammoura A, Touze E, Oppenheim C, Trystram D, Mas JL. Reversible angiopathy and encephalopathy after blood transfusion. J Neurol. 2003;250(1):116-118.
doi pubmed - Heo K, Park S, Lee JY, Lee BI, Lee SK. Post-transfusion posterior leukoencephalopathy with cytotoxic and vasogenic edema precipitated by vasospasm. Cerebrovasc Dis. 2003;15(3):230-233.
doi pubmed - Kawano H, Suga T, Terasaki T, Hashimoto Y, Baba K, Uchino M. [Posterior encephalopathy syndrome in two patients after cancer surgery with transfusion]. Rinsho Shinkeigaku. 2004;44(7):427-431.
pubmed - Huang YC, Tsai PL, Yeh JH, Chen WH. Reversible posterior leukoencephalopathy syndrome caused by blood transfusion: a case report. Acta Neurol Taiwan. 2008;17(4):258-262.
pubmed - Sato Y, Hirose M, Inoue Y, Komukai D, Takayasu M, Kawashima E, Koiwa F, et al. Reversible posterior leukoencephalopathy syndrome after blood transfusion in a patient with end-stage renal disease. Clin Exp Nephrol. 2011;15(6):942-947.
doi pubmed - Wada K, Kano M, Machida Y, Hattori N, Miwa H. Posterior reversible encephalopathy syndrome induced after blood transfusion for severe anemia. Case Reports in Clinical Medicine. 2013;2:332-334.
doi
This is an open-access article distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
