| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website http://www.neurores.org |
Case Report
Volume 2, Number 1, February 2012, pages 30-32
Is it Post-Thrombolysis Intracranial Hemorrhage?
Prakash R Paliwala, Hock L Teoha, Eric YS Tinga, Vijay K. Sharmaa, b
aDivision of Neurology, National University Hospital, Singapore
bCorresponding author: Vijay K Sharma, Division of Neurology, National University Hospital, 5 Lower Kent Ridge Road, 119074, Singapore
Manuscript accepted for publication February 14, 2012
Short title: Post-Thrombolysis Intracranial Hemorrhage
doi: https://doi.org/10.4021/jnr83w
| Abstract | ▴Top |
Intracranial hemorrhage is the commonest cause of hyperdensity on the non-contrast brain CT after thrombolysis with IV-TPA. This may range from minor petechial spots within the infarcted tissue to an extensive parenchymal hematoma. We present a patient who showed considerable clinical recovery after intravenous thrombolysis for acute ischemic stroke. However, his post-thrombolysis CT scan of the brain revealed a discrete hyperdensity in the infarcted region, due to extravasation of radio-contrast injected for CT angiography. His underlying end-stage renal failure probably contributed to a reduced rate of clearance of the contrast from his body.
Keywords: Brain CT; Intracranial hemorrhage; Thrombolysis; Radio-contrast
| Introduction | ▴Top |
New hyperdensity noted on the non-contrast computerized tomography (CT) imaging of the brain performed on day 2 after intravenous thrombolysis for acute ischemic stroke (AIS) is considered to represent intracranial hemorrhage (ICH). This de-novo finding often affects the treatment for such cases, especially regarding antithrombotic medications for secondary prevention of ischemic stroke. We describe the clinical and imaging findings in a patient who achieved significant clinical recovery after intravenous thrombolysis for AIS. However, the follow up CT scan of the brain on day 2 showed hyperdensity in the region of ischemic infarct that appeared like ICH.
| Case Report | ▴Top |
A 71-year-old Chinese male, presented with history of right-sided weakness for 2-hours. He had been taking medications for diabetes mellitus and hypertension. Furthermore, he was on maintenance hemodialysis for end-stage renal failure (ESRF) for 2-years.
On examination, his blood pressure was 176/90 mmHg and he was aphasic with fixed left-gaze. Severe weakness (power 0/5) was noted in right extremities and the National Institute of Health Stroke Scale (NIHSS) score was 19-points. Non-contrast computerized tomography (CT) showed hyperdense left middle cerebral artery (MCA) (Fig. 1A) and occluded left MCA was seen on CT angiography (CTA) (Fig. 1B). Intravenous tissue plasminogen activator (IV-TPA), initiated at 165-minutes after symptom-onset resulted in significant recovery (NIHSS at 24-hours reduced to 7-points).
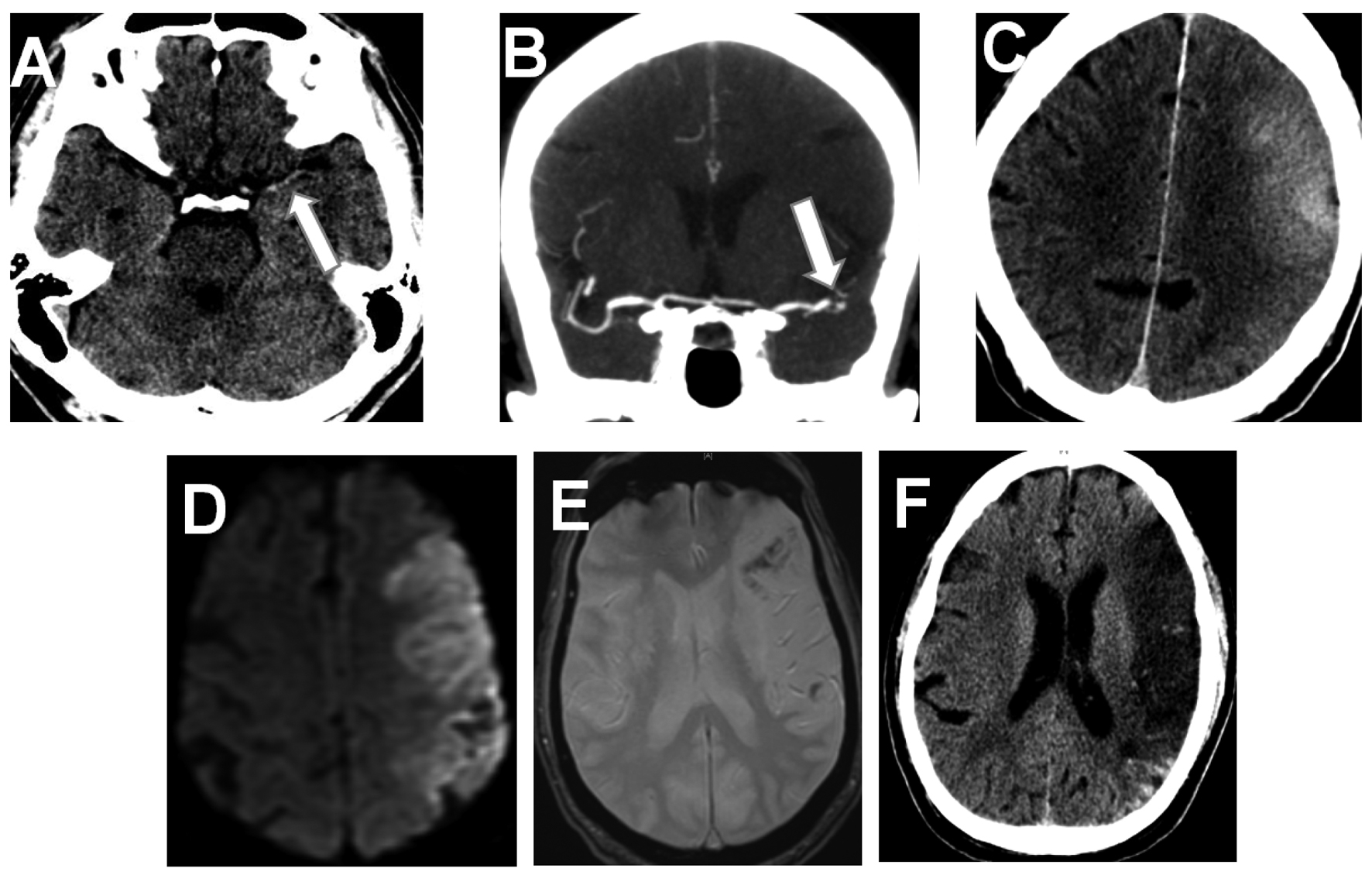 Click for large image | Figure 1. Pre-thrombolysis non-contrast brain CT shows a hyperdense left middle cerebral artery (MCA) (A). CT angiography shows Left MCA occlusion (B). Note the discrete left MCA hyperdensity on non-contrast CT, performed on day-2 (C). Diffusion-weighted brain-MRI, performed on day 2, shows acute left MCA infarction (D). Only a small area of hemorrhagic transformation is noted in the infracted region (E). Note the established left MCA infarction and disappearance of the hyperdensity on brain CT performed on day 7 (F). |
Interestingly, a discrete hyperdensity was observed on the follow-up non-contrast brain CT performed on day 2 (Fig. 1C). This was presumed as IV-TPA induced intracranial hemorrhage (ICH) and prompted us delaying the initiation of anti-thrombotic therapy. Magnetic resonance imaging (MRI) was performed for further evaluation within 4-hours of the brain CT. Diffusion-weighted imaging showed areas of restricted diffusion (Fig. 1D) in the left MCA territory. However, only a small area in the region of infarction demonstrated hemorrhagic transformation (Fig. 1E), and could not explain the hyperdensity observed on the CT scan (Fig. 1C).
| Discussion | ▴Top |
Arterial recanalization after thrombolysis often result in better clinical outcome [1]. However, sudden recanalization might cause reperfusion injury in some patients as considerable cerebral edema or ICH [2]. Cerebral ‘reperfusion injury’ may be asymptomatic or result into clinical deterioration, convulsions and altered consciousness. However, subsequently performed CT perfusion showed normal cerebral perfusion. Coupled with considerable recovery in our patient, normal CT perfusion excluded the possibility of ‘reperfusion injury’ as the cause of hyperdensity noted on brain CT performed on day 2.
IV-TPA may cause some neurotoxicity, especially in patients with prolonged ischemia, leading to an increased permeability of the blood brain barrier and contrast-extravasation or enhacement of the infract [3, 4]. Previous studies reported contrast extravasation after intraarterial thrombolysis or endovascular interventions [3, 4]. However, this phenomenon is observed when CT scan of the brain is performed within a short period after radio-contrast injection. Interestingly, the hyperdensity in our patients was seen on the CT scan performed about 22 hours after contrast injection that was administered intravenously. Although, it is difficult to substantiate, we hypothesize that ischemia-induced cerebral injury disrupted the blood brain barrier, leading to parenchymal extravasation of the radio-contrast. Renal failure in our patients further contributed to the delayed clearance of radio-contrast injected on day 1. He continued to improve despite a large cerebral infarction and CT hyperdensity disappeared on the CT scan performed on day-7 (Fig. 1F).
Conclusion
Our case serves as a reminder that hyperdensity noted on brain CT after IV-TPA should not be presumed as ICH, especially in patients who had received radio-contrast during few days prior to brain imaging.
Authors’ Contributions
All the authors have contributed significantly to this manuscript. Authors do not have any conflicts of financial interest.
| References | ▴Top |
- Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med. 1995;333(24):1581-1587.
pubmed doi - Yang GY, Betz AL. Reperfusion-induced injury to the blood-brain barrier after middle cerebral artery occlusion in rats. Stroke. 1994;25(8):1658-1664; discussion 1664-1655.
pubmed - Yoon W, Seo JJ, Kim JK, Cho KH, Park JG, Kang HK. Contrast enhancement and contrast extravasation on computed tomography after intra-arterial thrombolysis in patients with acute ischemic stroke. Stroke. 2004;35(4):876-881.
pubmed doi - Kastrup A, Groschel K, Ringer TM, Redecker C, Cordesmeyer R, Witte OW, Terborg C. Early disruption of the blood-brain barrier after thrombolytic therapy predicts hemorrhage in patients with acute stroke. Stroke. 2008;39(8):2385-2387.
pubmed doi
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
