| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website http://www.neurores.org |
Original Article
Volume 10, Number 3, June 2020, pages 73-79
Biomechanical Motion Analysis of Cervical and Thoracolumbar Spine During Ambulance Transport: A Healthy Volunteer Study
David A. Wamplera, d, Ronald M. Stewarta, Rena Summersb, Randall Schaeferb, Lawrence Roakesb, Craig Cooleya, Mike Shownc, Tasia Longb, Chetan Kharoda, Brian Eastridgea
aUT Health Science Center San Antonio, San Antonio, TX, USA
bSouthwest Texas Regional Advisory Council, San Antonio, TX, USA
cSchertz Emergency Medical Services, Schertz, TX, USA
dCorresponding Author: David Wampler, UT Health San Antonio, Department of Emergency Health Sciences, 4201 Medical Dr. Suite 120, San Antonio, TX 78229, USA
Manuscript submitted April 1, 2020, accepted April 14, 2020, published online May 30, 2020
Short title: Biomechanical Motion During Ambulance Transport
doi: https://doi.org/10.14740/jnr587
| Abstract | ▴Top |
Background: Recent evidence suggests that long spine board (LSB) may do little to manage spinal motion, and pose increased risk. This project sought to measure cervical and thoracolumbar motion during ambulance transport. The hypothesis was transport on a mattress with the head elevated without the LSB would allow less spinal movement than transport on an LSB.
Methods: A randomized healthy volunteer crossover trial measured spinal motion using biometric sensors. Positions analyzed included 0 and 10° on LSB. Stretcher alone with head elevated to 10°, 30°, 45° and 60°, with and without head blocks. Simulated ambulance transport was on city streets at or below posted speed limits.
Results: Nine subjects were included, with 66% being male. For cervical movement, there was no difference in axial, flexion/extension, or rotation (0.2 ± 0.1 mm vs. 0.2 ± 0.1 mm, 24 ± 12 mm vs. 22 ± 10 mm, and 5.1 ± 19° vs. 5.8 ± 20°, respectively). There were significant differences in lateral (3.7 ± 7 mm LSB vs. 2.0 ± 5 mm no LSB) movement and volumetric movement of the head (120 ± 172 mm3 LSB vs. 77 ± 86 mm3 no LSB). Positions allowing the lowest mean cervical volume of head movement were bed elevated to 30° and 45° with head blocks, (20 ± 22 mm3 and 12 ± 6 mm3, respectively). For thoracolumbar movement, there was no statistical difference in three-dimensional volumetric movement of the thoracolumbar spine (2 ± 0.6 mm3 LSB vs. 4.7 ± 5 mm3 no LSB).
Conclusion: Spinal motion was small in all groups. The stretcher mattress without LSB allowed less cervical motion than the LSB. Subjects secured to a stretcher mattress with head of the bed elevated to 30° had the least spinal movement.
Keywords: Spinal motion restriction; Prehospital medicine; EMS transport
| Introduction | ▴Top |
Since J. D. Farrington first formally described the long spine board (LSB) in “Death in a Ditch” [1], emergency medical services (EMS) providers have used this medical device during extrication and transport of trauma victims. The immobilization process is intended to hold the head in line with the torso to prevent secondary injury to the neural tissue that would normally be protected by the healthy spinal column. Historically, EMS providers have used an LSB during treatment and transport of any patient at risk for cervical spine injury. Despite the ubiquitous use of the LSB, there is a paucity of data documenting its safety and efficacy.
Complications related to the use of the LSB as an immobilization device may lie in its design. The LSB consists of a smooth, hard, flat surface with a low coefficient of friction. Specifically, the flat design offers no support for the natural lordotic curvatures of the human spine, likely a contributor to the discomfort and pain [2] patients experience, particularly during protracted transports from the field or between medical facilities.
In addition to pain, LSB utilization has been associated with increased anxiety following a traumatic event, cutaneous pressure ulceration [2], elevated intracranial pressure [3] and increased difficulty with airway management [4]. Likewise, use of the LSB may lead to unnecessary diagnostic imaging, as providers may have difficulty distinguishing if pain results from initial traumatic injury or from the patient being secured to the LSB for an extended period of time [5]. There is also a body of data that indicates LSB use in some trauma patients may actually be harmful [6, 7].
In contrast, modern ambulance stretchers have a padded mattress designed to conform to a patient’s anatomy. The stretcher mattress is designed for comfort, with a higher coefficient of friction, and demonstrated superiority in reducing patient movement over the LSB [8]. To date, there have been no randomized controlled trials of spinal immobilization strategies for the transport of trauma patients [9].
Furthermore, there is little evidence to support the optimal elevation levels for the head of the stretcher during prehospital transport. The contemporary critical care and neurosurgery literature suggest that intensive care patients suffering from traumatic brain injury should have the head of the hospital bed elevated to 30° as a therapeutic adjunct to control intracranial pressure and to minimize complications of aspiration [3, 10]. However, a Cochrane review in 2017 called into question the literature supporting this standard practice and recommended clinical outcome trials to be conducted to validate this practice [11].
A previous publication looking at the lateral motion on and off the LSB on an EMS stretcher [8] used analog measurement to determine lateral motion. Current technology allows for the accurate three-dimensional (3D) biomechanical analysis of complex human movement. In light of the paucity of evidence supporting the use of the LSB as an immobilization device for the management and transport of the potentially spinally injured patient [12], this study was developed with the following goals: to evaluate the biomechanical motion of the spine on the padded EMS stretcher compared to the LSB and to evaluate the biomechanical impact of the elevation of the head of the EMS stretched on spinal movement during transport.
| Materials and Methods | ▴Top |
Study design
This was a randomized 10-sequence crossover biomechanical analysis of nine healthy volunteers. Body movement was recorded while each participant was transported by ambulance in various spinal immobilization conditions. Comparisons included participant’s body movements (cervical, torso, thoracolumbar and pelvic) while immobilized on LSB with cervical collar (c-collar) and head blocks to body movement when placed directly on a stretcher alone both with and without c-collar and head blocks, in different head of stretcher elevations.
Instrumentation
Each participant underwent full informed consent, and their height and weight measurements were taken. Participants were fitted into full bodysuits with integrated Xsens (Xsens North America Inc., Culver City, CA) motion analysis technology, including 17 accelerometers which were secured to the following anatomical areas: forehead (via headband), neck, upper chest, abdomen, waist, thighs, calves, ankles, arms, forearms and hands (Fig. 1). Accelerometers were calibrated against the anatomical position. Inertial sensors facilitated the accurate kinematic measurement, using 17 wireless motion trackers for full-body human motion measurements. The system utilized the following four steps to estimate 3D joint angles: 1) definition of segment anatomical frame axes and segment lengths; 2) sensor to segment anatomical frame alignment; 3) relation of segment with global frame and 4) relation of two adjacent segments. Body position and force vector data were continuously streamed at a rate of 50 Hz to a laptop computer running the manufacturer software.
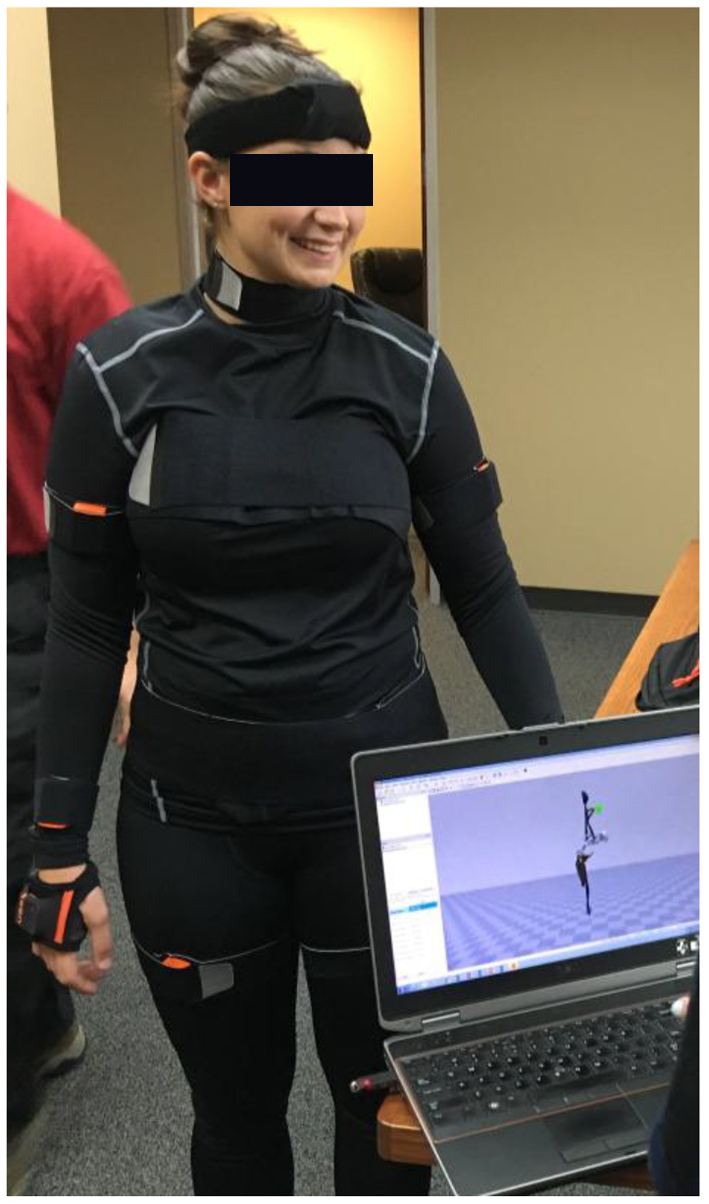 Click for large image | Figure 1. Model of the system used for measurement (including 16 accelerometers that communicate wirelessly), and the laptop interface. |
Participant vital signs, including heart rate, blood pressure, blood oxygen saturation, respiratory rate and electrocardiogram, were monitored throughout each transport using a cardiac monitor with vital sign capability.
Transport conditions
A type III ambulance and a Stryker Power-PRO XT Ambulance Cot were used during the study. The driver was a professional paramedic and was blinded (closed partition) to randomized participant positioning. Transport time as 8 ± 1.5 min. Transport positions included: supine with the LSB at 0°, and supine with the LSB tilted head up to 10°, both with c-collar and foam head blocks (Fig. 2a). Transport conditions without the LSB included: supine with head of stretcher elevated 10°, 30° (Fig. 2b and c), 45° and 60°. Each head of stretcher position without the LSB was tested with and without rigid c-collar and lightweight foam head blocks. When c-collar and head blocks were used, they were secured to the stretcher with medical tape.
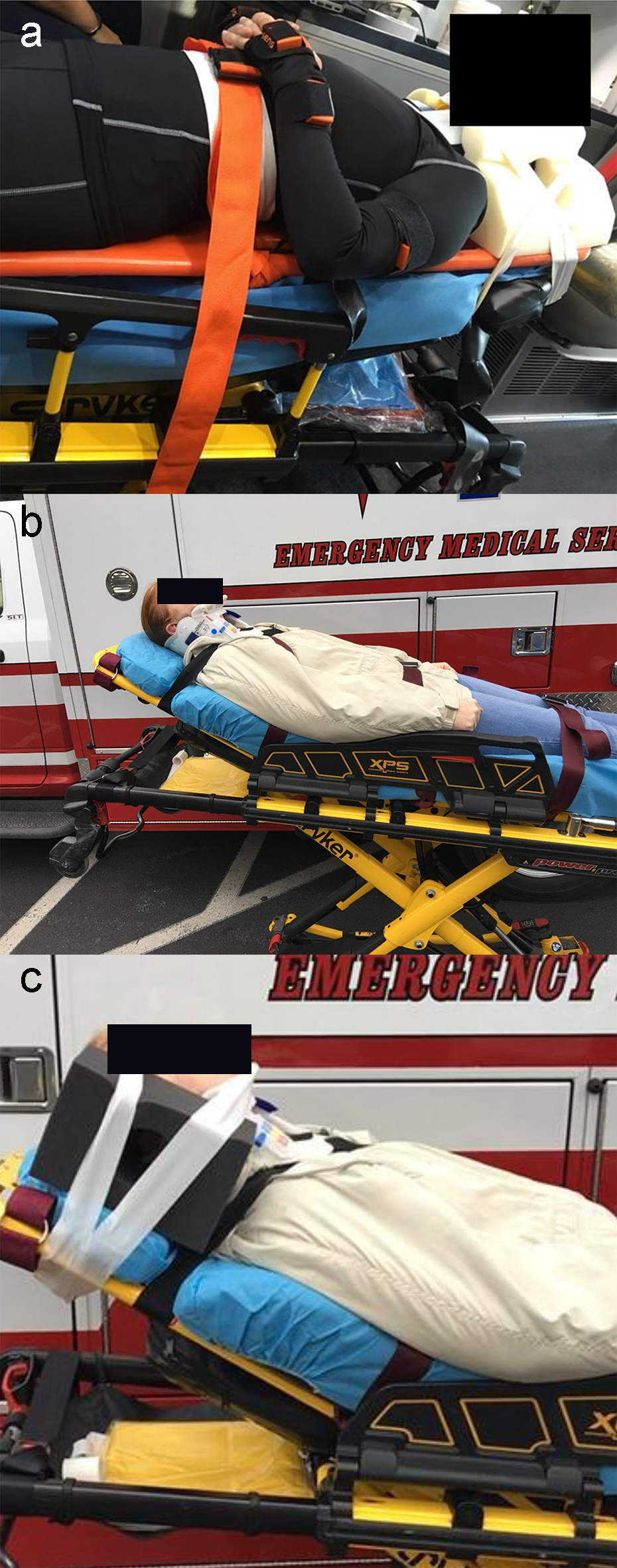 Click for large image | Figure 2. (a) An example of a subject secured to a long spine board on the EMS stretcher with the head of the bed elevated to 10°. (b) Example of a subject secured to the stretcher with cerical collar without head blocks with the head of the bed elevated to 30°. (c) Example of a subject secured to the stretcher with cerical collar and head blocks with the head of the bed elevated to 30°. |
Once the participant was secured in the appropriate position according to the randomization scheme, data collection was initialized, and the driver drove a predetermined route on city streets. The route included five right turns, four left turns, two looping turns and two speed bumps.
Data collection and analysis
Motion data were abstracted from the proprietary software into spread sheets, and the data were transferred to an independent analysis service (Guidance Engineering, Seattle, WA) for analysis. Engineers were blinded to the study hypothesis.
For measurement of cervical motion, the motion of the head accelerometer device was compared only to the torso device; the torso was virtually anchored, and motion of the head was relative to a stationary torso. Likewise, for the thoracolumbar motion, the torso was virtually anchored, and the pelvic device motion was utilized. Volumetric motion was defined as the overall amount of space that one of the accelerometer devices occupied as a function of the thoracic accelerometer device.
Descriptive statistics were used for demographic and ordinal data; t-test was used to infer differences between transport positions; Chi-square was used for categorical data. In all cases statistical significance was defined as a P-value less than 0.05.
| Results | ▴Top |
Nine participants volunteered for this study, mean age was 36 years (95% confidence interval (CI): 27 - 45 years), mean body mass index (BMI) was 25 (95% CI: 23.1 - 28.1) and 66% were males. For cervical movement in the supine patient, there was no difference in axial, flexion/extension or rotation (0.2 ± 0.1 mm vs. 0.2 ± 0.1 mm, 24 ± 12 mm vs. 22 ± 10 mm and 5.1 ± 19° vs. 5.8 ± 20°, respectively) when comparing LSB versus stretcher. There were significant differences in lateral (3.7 ± 7 mm LSB vs. 2.0 ± 5 mm no LSB) movement and volumetric movement of the head (120 ± 172 mm3 LSB vs. 77 ± 86 mm3 no LSB).
Positions allowing the lowest mean cervical volume of head movement were head of stretcher elevated to 30° and 45° with head blocks (20 ± 22 mm3 and 12 ± 6 mm3, respectively) (Fig. 3).
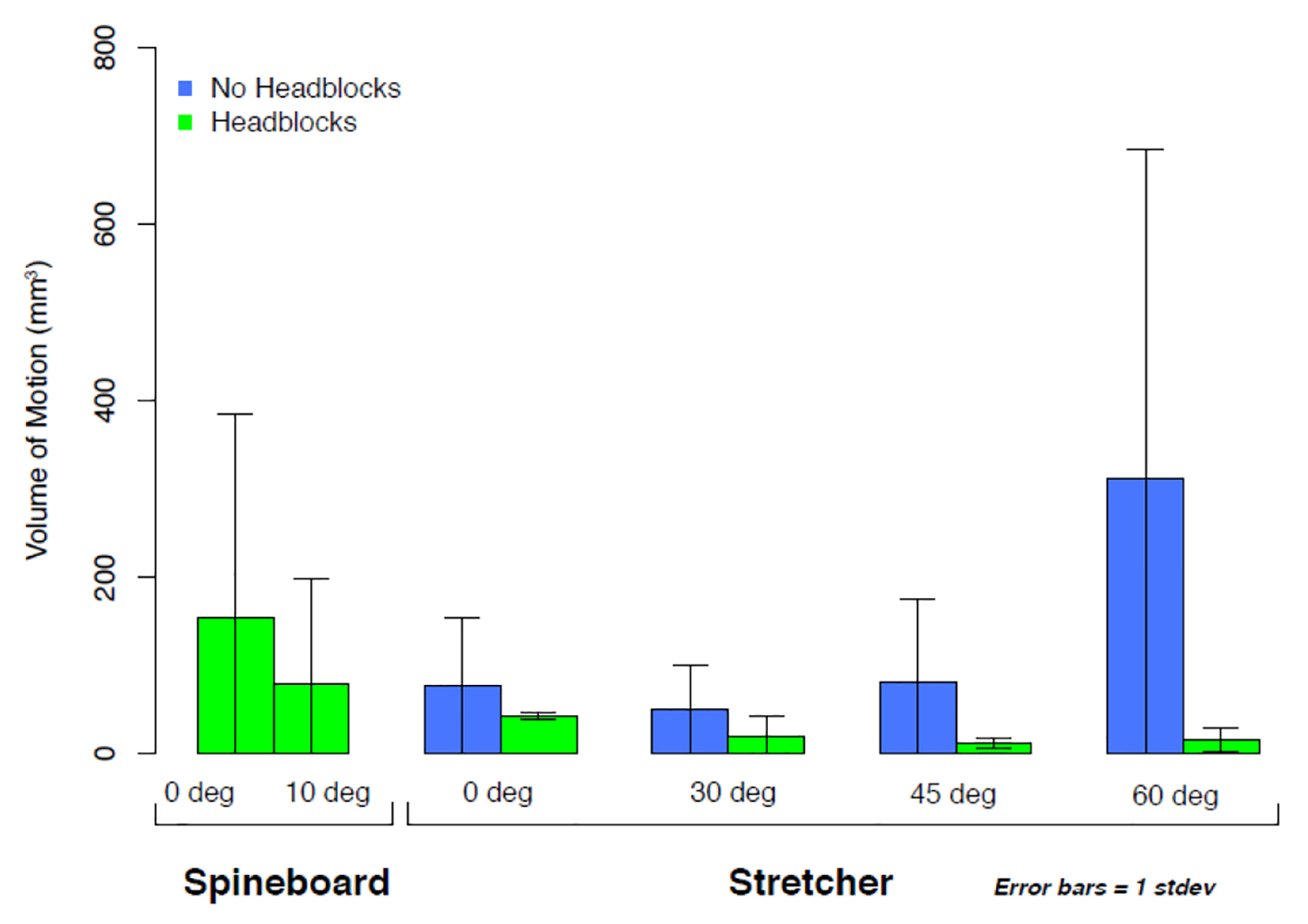 Click for large image | Figure 3. Bar graph with error bars of the total volumetric motion of the head relative to the torso. All subjects were fitted with a cervical collar during transport. All subjects on long spine board were also fitted with head blocks secured to the long spine board. Stretcher subjects were transported either with or without head blocks, and all transports were 8 min in duration. |
For thoracolumbar movement, there was no statistical difference in 3D volumetric movement of the thoracolumbar spine (2 ± 0.6 mm3 LSB vs. 4.7 ± 5 mm3 no LSB) (Fig. 4).
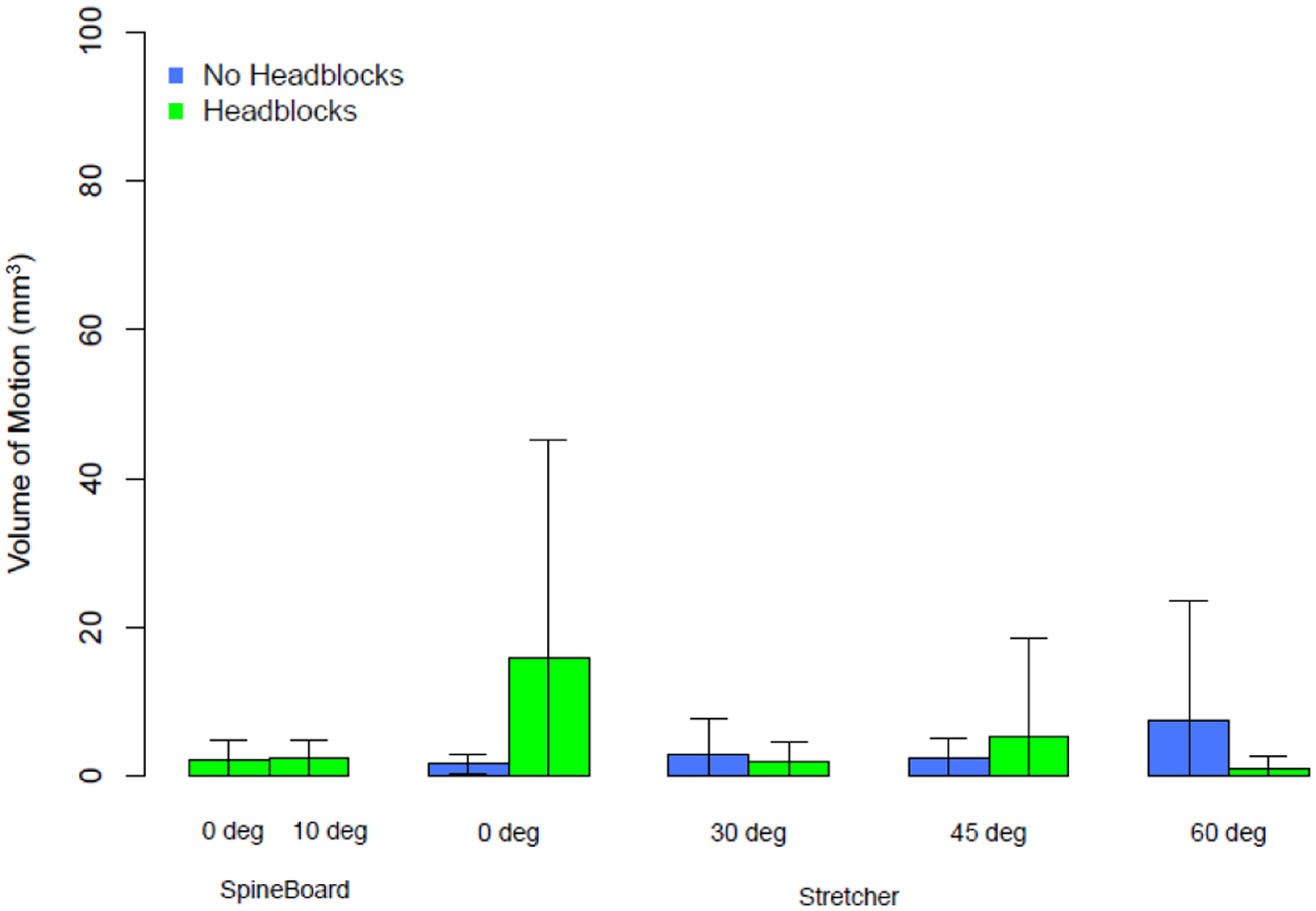 Click for large image | Figure 4. Bar graph with error bars of the total volumetric motion of the upper 10% of the thigh relative to the torso, all transports were 8 min in duration. |
For vital signs monitoring, the mean blood pressures and heart rates are described in Table 1. There were no differences in vital signs to include pain level when comparing to the supine patient on LSB versus stretcher.
 Click to view | Table 1. Changes in Vital Signs |
| Discussion | ▴Top |
This study precisely measures movement at the level of the head compared to the torso during ambulance transport with and without LSB and with the head of the stretcher elevated to various positions. By measuring the relative movement of the head (i.e. cervical motion), and movement of the hip (i.e. thoracolumbar), as compared to the torso during ambulance transport of healthy volunteers, the effect of spinal immobilization with the LSB was evaluated. In all scenarios, the participants had greater volumetric motion on the LSB than they did on the stretcher mattress alone.
Using the same biometric measurement technology and similar supine transport conditions, Thezard et al demonstrated reduced angular displacement and increased linear displacement in the supine patient on an LSB with c-collar and head blocks as compared to the supine patient with c-collar alone [13]. These data are consistent with observations in this paper, but with the inclusion of head blocks motion was less without the LSB. Furthermore, with the head of bed elevation motion was further reduced in the 30 - 45° range.
Based on our results, the head of stretcher elevated to 30° may be the optimal position to minimize movement. We speculate that this may be because the 30° angle still allows significant weight to be distributed along the stretcher mattress. Even during hard ambulance breaking events, the elevation preserves a more normal body position and hemodynamics of blood flow into, and out of, the head [14]. In addition, although not specifically shown in this study, this position would be expected to be more comfortable for most patients when compared to the LSB. While there is concern that sitting the potentially spine injured patient too upright may induce significant downward force on the spine and exacerbate existing injuries, it is interesting to note that small movements are detected in all positions except for head of stretcher elevated to 60°, which had much higher movement. While there is no significant information on the tolerable amount of safe cervical motion, it is likely that some cervical motion is tolerable [8, 15]. Our results demonstrate that the LSB had more movement of the neck to the torso when compared to a modern ambulance stretcher. The clinical importance of this finding is unclear as our study cohort did not have spinal column injury. The LSB may still have utility as an extrication tool to carry patients short distances by foot from the exact site of the injury.
Limitations
This is a nonclinical, healthy volunteer study of uninjured participants; therefore, participants did not self-splint or experience significant pain upon movement unlike a patient who has experienced a traumatic injury. Likewise, it is unclear if spinal column injuries would produce more volumetric movement during transport, especially those with mechanically unstable fracture patterns. The sample size is small, but the frequency of data point capture (50 Hz) resulted in a very large dataset, with each of nine patients undergoing an average of 8-min transport per position.
Conclusion
Based upon this study’s findings, we submit that the optimal transport modality is on stretcher with head blocks and head of stretcher elevated to 30°.
Acknowledgments
None to declare.
Financial Disclosure
Research reported in this presentation was funded through a United States Department of Defense Grant Award (W81XWH-14-2-0149).
Conflict of Interest
All authors report no conflict of interest.
Informed Consent
Each participant underwent full informed consent.
Author Contributions
DW: study design and manuscript preparation. DW, RMS, RSum, RSch, TL, CC, MS, CK, BE and LR: data management.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Farrington JD. Death in a ditch. Bulletin - American College of Surgeons 1967:121-130.
- Morris CG, McCoy EP, Lavery GG. Spinal immobilisation for unconscious patients with multiple injuries. BMJ. 2004;329(7464):495-499.
doi pubmed - Feldman Z, Kanter MJ, Robertson CS, Contant CF, Hayes C, Sheinberg MA, Villareal CA, et al. Effect of head elevation on intracranial pressure, cerebral perfusion pressure, and cerebral blood flow in head-injured patients. J Neurosurg. 1992;76(2):207-211.
doi pubmed - Crosby ET, Lui A. The adult cervical spine: implications for airway management. Can J Anaesth. 1990;37(1):77-93.
doi pubmed - March JA, Ausband SC, Brown LH. Changes in physical examination caused by use of spinal immobilization. Prehosp Emerg Care. 2002;6(4):421-424.
doi pubmed - Hauswald M, Ong G, Tandberg D, Omar Z. Out-of-hospital spinal immobilization: its effect on neurologic injury. Acad Emerg Med. 1998;5(3):214-219.
doi pubmed - Haut ER, Kalish BT, Efron DT, Haider AH, Stevens KA, Kieninger AN, Cornwell EE, 3rd, et al. Spine immobilization in penetrating trauma: more harm than good? J Trauma. 2010;68(1):115-120; discussion 120-111.
doi pubmed - Wampler DA, Pineda C, Polk J, Kidd E, Leboeuf D, Flores M, Shown M, et al. The long spine board does not reduce lateral motion during transport - a randomized healthy volunteer crossover trial. Am J Emerg Med. 2016;34(4):717-721.
doi pubmed - White CCt, Domeier RM, Millin MG, Standards, Clinical Practice Committee NAoEMSP. EMS spinal precautions and the use of the long backboard - resource document to the position statement of the National Association of EMS Physicians and the American College of Surgeons Committee on Trauma. Prehosp Emerg Care. 2014;18(2):306-314.
doi pubmed - Ng I, Lim J, Wong HB. Effects of head posture on cerebral hemodynamics: its influences on intracranial pressure, cerebral perfusion pressure, and cerebral oxygenation. Neurosurgery. 2004;54(3):593-597; discussion 598.
doi pubmed - Alarcon JD, Rubiano AM, Okonkwo DO, Alarcon J, Martinez-Zapata MJ, Urrutia G, Bonfill Cosp X. Elevation of the head during intensive care management in people with severe traumatic brain injury. Cochrane Database Syst Rev. 2017;12:CD009986.
doi pubmed - Fischer PE, Perina DG, Delbridge TR, Fallat ME, Salomone JP, Dodd J, Bulger EM, et al. Spinal motion restriction in the trauma patient - a joint position statement. Prehosp Emerg Care. 2018;22(6):659-661.
doi pubmed - Thezard F, McDonald N, Kriellaars D, Giesbrecht G, Weldon E, Pryce RT. Effects of spinal immobilization and spinal motion restriction on head-neck kinematics during ambulance transport. Prehosp Emerg Care. 2019;23(6):811-819.
doi pubmed - Schulz-Stubner S, Thiex R. Raising the head-of-bed by 30 degrees reduces ICP and improves CPP without compromising cardiac output in euvolemic patients with traumatic brain injury and subarachnoid haemorrhage: a practice audit. Eur J Anaesthesiol. 2006;23(2):177-180.
doi pubmed - Swartz EE, Nowak J, Shirley C, Decoster LC. A comparison of head movement during back boarding by motorized spine-board and log-roll techniques. J Athl Train. 2005;40(3):162-168.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
