| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://www.neurores.org |
Original Article
Volume 14, Number 1, June 2024, pages 1-7
Small Number of Coils With Extended Length in the Endovascular Treatment of Cerebral Aneurysm: Experience of 108 Cases in a Single-Center
Bambang Tri Prasetyoa, Beny Riliantoa, b, Ricky Gusanto Kurniawana
aNeurointervention Division, Mahar Mardjono National Brain Center Hospital, East Jakarta, Indonesia
bCorresponding Author: Beny Rilianto, Neurointervention Division, Mahar Mardjono National Brain Center Hospital, East Jakarta, Indonesia
Manuscript submitted February 12, 2024, accepted May 3, 2024, published online May 25, 2024
Short title: Coils in the Cerebral Aneurysm
doi: https://doi.org/10.14740/jnr777
| Abstract | ▴Top |
Background: Knowledge about the number and packing density of coils for aneurysm treatment affects the efficiency of health services and hospital financing. This study aimed to report case series with a small number of coils with longer lengths and impact on packing density.
Methods: We retrospectively analyzed the morphology of aneurysms (location and size) and the data of characteristic features of coils (numbers, diameter size, length, and packing density) from the cerebral aneurysm registry at a single center from January 2019 to June 2022. Kruskal-Wallis analysis was performed to identify the association between coil characteristics based on the size of the aneurysm.
Results: Of the 108 patients included in the study, 116 aneurysms were identified and coiled; 66 were small (< 5 mm), 42 were moderate (5 - 10 mm), and eight were large (> 10 mm). Most cases utilized framing first coil (in 64.65%) and helical coils (in 31.89%). The total length of framing coils (< 5 mm: 6.76 ± 4.14 cm, 5 - 10 mm: 11.28 ± 6.93 cm, > 10 mm: 29.33 ± 12.59 cm) and helical coils (< 5 mm: 5.95 ± 2.82 cm, 5 - 10 mm: 11.66 ± 7.3 cm, > 10 mm: 22.32 ± 11.48 cm) also increased with group size. The highest packing density (46.70%) was achieved in small aneurysms (< 5 mm).
Conclusion: In small aneurysm, one to three coils per aneurysm were required to achieve tight coil packing density by extending the length of coil.
Keywords: Coil embolization; Packing density; Cerebral aneurysm; Coil number; Coil length
| Introduction | ▴Top |
Endovascular treatment for intracranial aneurysms has grown in recent years. Its goal is to form occlusion of the aneurysm, either complete or near complete. Studies have established that endovascular treatment offers lower risk of mortality and shorter hospitalization time. Aneurysm size, location, patient’s medical history, and operator’s experience are important factors to consider when performing endovascular treatment [1, 2]. Coil embolization is a standard endovascular treatment for aneurysms, especially for narrow-neck aneurysms, which entails filling the aneurysm sac with coils [3]. Fewer neurological complications associated with the procedure make endovascular coiling the most common treatment for aneurysms [4, 5].
In addition, coil packing density of at least 20% to 25% is known to be important for preventing recanalization following endovascular coiling [6]. However, coil embolization carries significant financial burden, and this is partly attributable to the coils themselves; the larger the aneurysm, the more coils needed, and, consequently, the higher the cost incurred [7, 8]. Despite this, most of the National Health Insurance in the developing countries does not provide full coverage of the costs associated with endovascular coiling. This is notable, as it means endovascular treatment remains financially inaccessible to many patients. On that account, knowledge on the appropriate number of coils needed in endovascular procedures, as well as coil packing density, is of paramount importance to ensure cost efficiency.
Therefore, this descriptive study aimed to report that a study a small number of coils with longer lengths could achieve good packing density at a tertiary comprehensive stroke center.
| Materials and Methods | ▴Top |
Ethics approval
Our retrospective study design and protocol were approved by the hospital’s research ethics committee (No. LB.02.01/KEP/068/2022). This study was conducted in compliance with the Declaration of Helsinki.
Inclusion criteria
Under institutional review board approval, we obtained data retrospectively from the cerebral aneurysm registry of the Indonesian largest comprehensive stroke center, Mahar Mardjono National Brain Center Hospital, East Jakarta between January 2019 and June 2022. We included all patients who underwent endovascular coiling. Patients with incomplete records (missing morphological data, coil profile) were excluded. We reviewed patients’ clinical characteristics (age, gender, vascular risk factors and mortality), aneurysmal morphology (location and size), and the characteristic features of coils (number, size, and packing density).
Angiography and aneurysmal morphology
The parameters of aneurysmal morphology analyzed in this study included aneurysmal location and size - neck (mm) and dome (mm), which were obtained with the biplane digital subtraction angiography (DSA) and 3D rotational angiography: the Philips Allura Xpert FD 20 X-ray system with 258° complex rotation scan. Aneurysm was classified based on site and size as follows: small (< 5 mm), medium (5 - 10 mm), and large (> 10 mm).
Endovascular coiling and packing density
In our center, two major coil brands were used in the endovascular procedure: Optima Coil System (Balt, France) and Axium Prime (Medtronic, USA). A combination of coil brands might be used in the same procedure. Coil embolization by four experienced operators (three interventional neurologists and one neurosurgeon) was performed on all cases (simple coiling) without the usage of balloons or stents, as wide-neck aneurysms were treated with surgical clipping in our institution. Complex or 3D-shaped coils were deployed as the initial framing coil, followed by helical coils as filling. Coiling was deemed adequate when sufficient occlusion of the aneurysm was seen angiographically. The number of coils placed and their packing density (%) - calculated with AngioCalc (Cerebral and Peripheral Aneurysm Calculator) [9] - were taken as data for analysis based on the morphology of the cerebral aneurysm and on the characteristics of the coils.
Statistical analysis
Data were analyzed and tabulated using the software STATA (version 17.0; StataCorp, Texas, USA). Subjects were divided into three groups, based on the aforementioned aneurysmal diameter classification (small, medium, and large). Coil features (number, size, length, and packing density) were obtained as numbers and presented as mean and standard deviation (SD). Since the size of the aneurysm that was used provided ordinal level data that are not normally distributed, all analyses in the present study were performed using Kruskal-Wallis to find differences between groups and established a P < 0.05 as the threshold of statistical significance, with 95% confidence intervals (CIs).
| Results | ▴Top |
We reported 130 patients treated with endovascular coiling, 22 patients were excluded due to incomplete data, and 108 patients were included in the study (eight patients have multiple aneurysm); 116 aneurysms were identified and coiled: 66 were small (< 5 mm), 42 were moderate (5 - 10 mm), and eight were large (> 10 mm) (Fig. 1). By age, the group of 50 - 59 years old was the most common in our study population, the mean was 53 years old (SD: 11.46), with female gender predominance (62%). Hypertension was the most frequently found vascular risk factor (78%) among patients, followed by dyslipidemia (34%) and diabetes mellitus (16%) (Table 1).
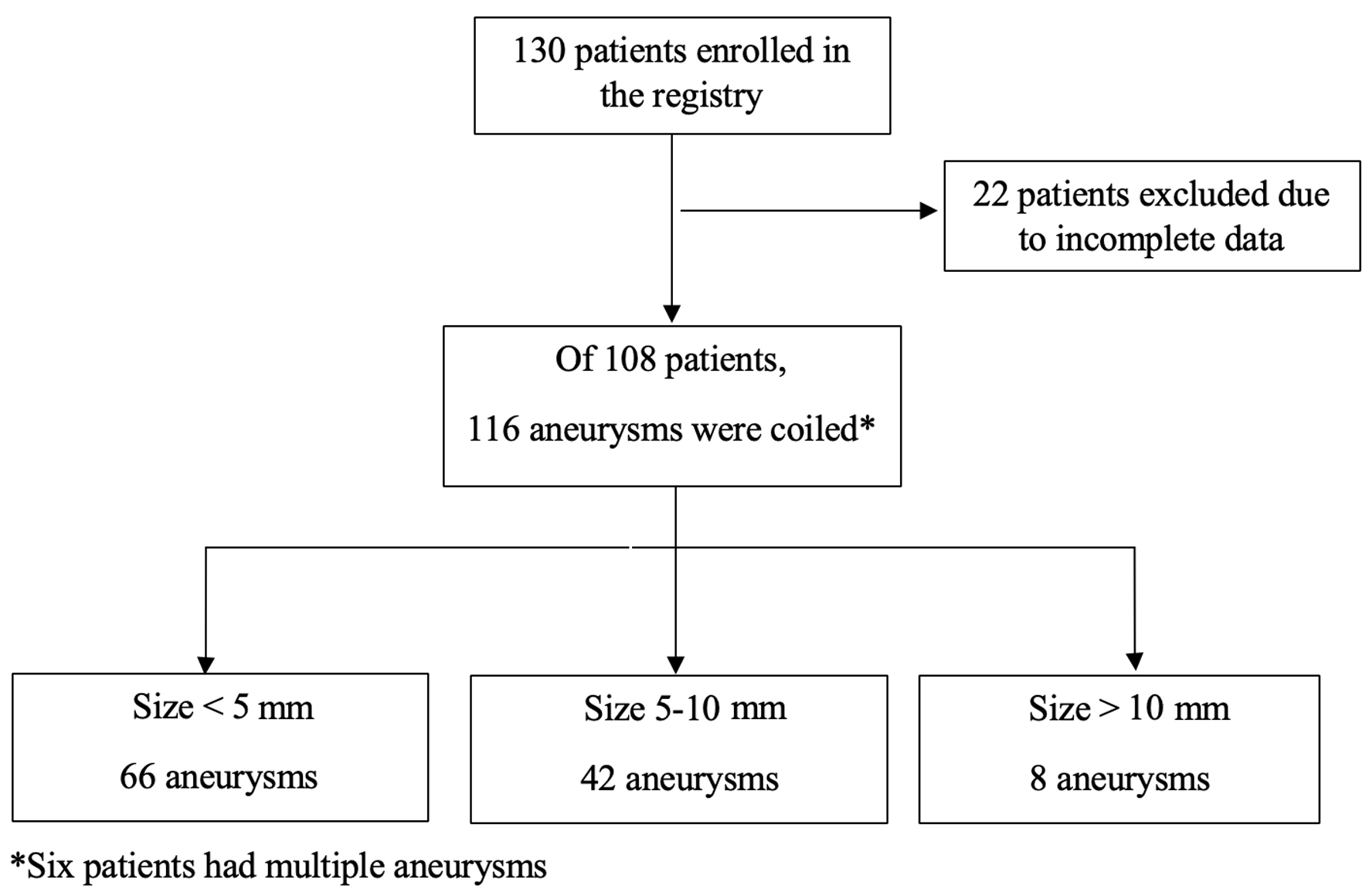 Click for large image | Figure 1. Patients flow diagram. |
 Click to view | Table 1. Clinical Characteristics of Patients |
Of the 108 patients, 116 aneurysms were identified and coiled. Most patients (n = 98; 84%) had ruptured aneurysms. Of the 116 aneurysms, 66 (57%) were small (< 5 mm), 42 (36%) were moderate (5 - 10 mm), and eight (7%) were large (> 10 mm). Mean neck size was 2.98 mm, while mean dome size was 5.09 mm. There were 85 aneurysms (75.3%) in the anterior circulation and most of the coiled aneurysms originated from the anterior communicating artery followed by the internal carotid artery, while in the posterior circulation, most aneurysms originated from the posterior communicating artery (Table 2).
 Click to view | Table 2. Location and Size of Aneurysms |
The coil was divided into two parts: framing and helical. Mean number of framing coils saw a slight increase with group size (< 5 mm: 0.86 ± 0.55, 5 - 10 mm: 0.97 ± 1.5, > 10 mm: 1.12 ± 1.64), but there was no statistically significant difference (P = 0.799). Mean diameter size of framing coil, however, increased considerably with group size (< 5 mm: 3.19 ± 1.01 mm, 5 - 10 mm: 4.64 ± 1.79 mm, > 10 mm: 9.67 ± 3.46 mm), and this was statistically significant (P = 0.015). Both helical coil’s number (< 5 mm: 1.5 ± 0.94, 5 - 10 mm: 2.52 ± 0.81, > 10 mm: 2.75 ± 1.9) and size (< 5 mm: 2.69 ± 1.03 mm, 5 - 10 mm: 4.17 ± 1.94 mm, > 10 mm: 7 ± 3.16 mm) increased with group size, with statistical significance (P < 0.001 for both). The total length of framing coil increased with group size (< 5 mm: 6.76 ± 4.14 cm, 5 - 10 mm: 11.28 ± 6.93 cm, > 10 mm: 29.33 ± 12.59 cm), and the total length of helical coil also increased with group size (< 5 mm: 5.95 ± 2.82 cm, 5 - 10 mm: 11.66 ± 7.3 cm, > 10 mm: 22.32 ± 11.48 cm). Packing density, meanwhile, tended to decrease with group size (< 5 mm: 46.70±3.15%, 5 - 10 mm: 33.06±0.26%, > 10 mm: 35.46±0.31%), with significant difference between groups (P < 0.001) (Table 3). In most of the treated aneurysms, only one coil (in 64.65% of cases) and more coils (in 31.89% of cases) were deployed. We provide a case illustration of a ruptured anterior communicating artery (ACoA) aneurysm in a patient treated with two coils: framing and helical coil (Fig. 2).
 Click to view | Table 3. Characteristic Features of Coils and Size of Aneurysms |
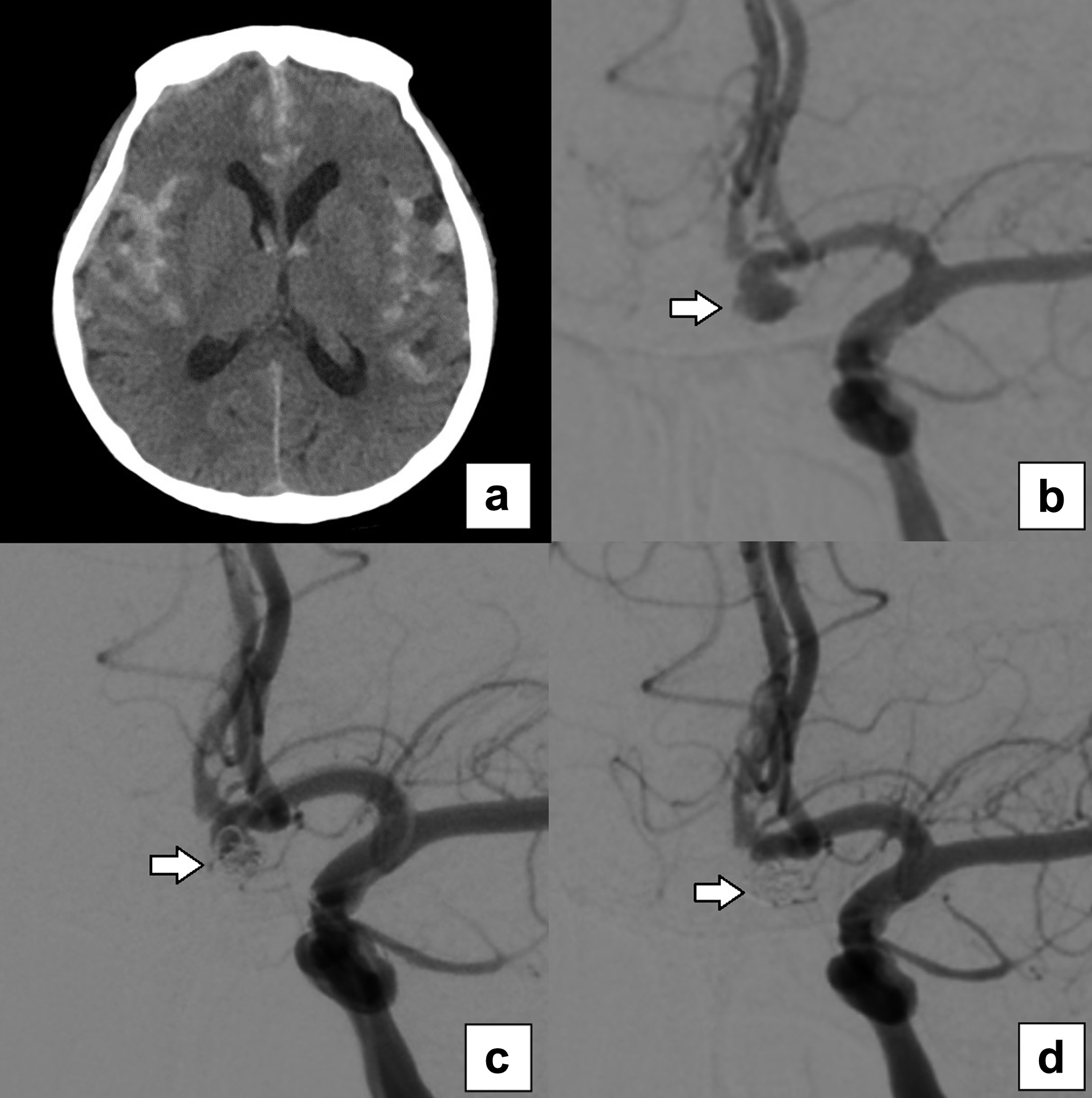 Click for large image | Figure 2. Case illustration of aneurysmal SAH of a 66-year-old female who underwent simple endovascular coiling. CT scan revealed a diffuse SAH (a). DSA showed a saccular cerebral aneurysm located in ACoA with neck 1.07 mm, dome 3.88 × 2.55 mm (arrow) (b). The first coil (4 mm × 10 cm framing coil) was inserted (c), followed by the second coil (3 mm × 10 cm helical coil) (arrow). Packing density was achieved by 30.53% (arrow) (d). ACoA: anterior communicating artery; CT: computed tomography; DSA: digital subtraction angiography; SAH: subarachnoid hemorrhage. |
| Discussion | ▴Top |
We reported that more than half (56.8%) of the cerebral aneurysms in our study had a size of less than 5 mm, with the anterior cerebral circulation as the most common site of origin. This is in coherence with studies conducted in Hong Kong, Singapore, as well as a previous Indonesian study [10-12]. Meanwhile, in Finland, ruptured aneurysms had an average size of 7 mm, and a Brazilian study reported that most aneurysms (67.7%) were between 5 and 10 mm [13, 14]. This suggests that Asian populations generally have smaller aneurysms than Western populations. As such, the number of coils necessitated in endovascular treatment may also vary between them.
In our study, both helical coil number and size increased with aneurysmal size (P < 0.001). However, while framing coil size increased with aneurysmal size (P = 0.015), framing coil number did not (P = 0.799), and most cases (64.65%) needed only one framing coil. In smaller aneurysm sizes, some treatments used helical coil without framing, significantly when the morphology was elongated shape. In other words, while larger aneurysms may need more helical coils, in most cases, adequate coiling was achievable with one framing coil and two helical coils, allowing for an average coil number of 1 - 3 in our experience, through larger coil size. Vanzin et al also found that the number of coils needed is directly proportional to the aneurysmal size. However, they reported an average number of coils of 8 per aneurysm [7].
The number of coils needed in the endovascular treatment of aneurysms is influenced by several factors, such as coil length, thickness, type, aneurysmal shape, as well as operator’s skill and experience [7, 15]. Endovascular treatment with larger coils can prevent failure in the complete occlusion of aneurysms, and a stiffer framing coil or a larger coil diameter can help prevent aneurysm recanalization [16, 17]. The percentage of framing coil from total coil volume has been demonstrated to be a statistically significant predictor of aneurysm recurrence post-coiling [18]. Using large-sized coil, Zhang et al were able to achieve similar occlusion rates while significantly decreasing the average number of coils per aneurysm to 2.98 ± 1.09 - a number similar to our finding - and lowering the recurrence rate at follow-up. They postulated the use of a large-sized coil as the initial embolization might be a new strategy for endovascular treatment [19]. The larger first coil has sufficient expansion and adhesion to the aneurysm inner wall, which is similar to the advantage provided by a flow-diverting stent with 30-35% surface area coverage [20, 21]. Kaesmacher et al also reported that aneurysmal occlusion using higher-volume coils led to the use of fewer coils - without a significant difference in the incidence of side effects - as well as higher packing density compared to when using lower-volume coils, thus leading to more complete aneurysm occlusion [22]. Our study confirmed these findings; we were able to achieve adequate occlusion of larger aneurysms with fewer framing coils by using larger-sized coils.
A higher packing density during unassisted coil embolization is linked to more long-lasting occlusion of the aneurysm [23, 24]. We found a mean packing density of 38.41% in occluded aneurysms in our study. Packing density differed significantly between group sizes (P < 0.001), tending to decrease with increasing aneurysmal size. Packing density has been shown to affect the recurrence of intracranial aneurysms, in addition to hemodynamic factors and vascular geometry [25]. Packing density more than 19% was the main predictor of complete occlusion of aneurysms [26]. In coherence, using computer-generated aneurysmal models to simulate hemodynamics, recurrent aneurysms had significantly lower coil packing density and higher uncoiled aneurysmal volume, the latter of which was an independent predictor for recurrence [3]. Vogler et al corroborated this, demonstrating a high success rate of occlusion from the use of high-packing density coils [27]. However, a study in Japan found that aneurysm volume (odds ratio (OR): 15.3; P < 0.001) and residual volume (OR: 30.9; P < 0.001) were significant predictors for recanalization, not packing density (OR: 0.98; P = 0.341) [6]. Furthermore, Lee et al also found no correlation between volume packing density and recanalization, and Piotin et al found no difference in the effect of coil packing density between patients who had recurrence and those who did not [28, 29]. Apart from the contradictory findings of the aforementioned studies, based on our research, high packing density influences the success of aneurysm occlusion based on the size of the aneurysm.
The higher cost of endovascular coiling was attributable to the more costly coil devices, when compared to clips [8, 30]. It stands to reason that extending the length of coils could be an effective strategy in decreasing total hospital costs. However, cost-reduction plans often enhance issues related to restricting the types of coils. The types, numbers of coils, and perceived efficacy have an impact on coil selection, but no studies have proven that a single coil is more efficacious than the other [31, 32].
In this study, we found that fewer number of coils, with extended size and high packing density, did not reduce the efficacy of treatment. That being the case, our findings may serve as a consideration for healthcare providers in Indonesia to determine the predictive value of the number of coils vis-a-vis their efficacy. The use of a minimum number of coils by extending the coil size may be an alternative strategy to maintain proper coil packing density. This approach could be applied if long-term durability is not a major problem, especially in older patients. However, in younger who require long-term durability, this strategy must be considered on a case-by-case basis.
Study limitations
Our study has limitations. It was conducted in a single center. In this study, the number of samples was only 116, which may not be generalized, especially for large aneurysms, which were only eight samples. However, in the small aneurysm group, the proportion is quite large. Furthermore, this is a descriptive study with no comparator or control group with a standard number of coils. This study is also limited to “narrow neck aneurysms” and “simple coiling”. Some interventionalists might take a different approach to using framing coils. Thus, further multicenter investigations with larger prospective and two arms are still needed as well as adequate follow-up to evaluate the perioperative complication and obliteration rate (Raymond-Roy occlusion classification).
Conclusion
This study found that fewer coils per aneurysm could achieve good packing density by extending the length, especially the smaller dome size. These strategies might be considered to provide cost-reduction with acceptable endovascular treatment of cerebral aneurysms.
Acknowledgments
The authors gratefully acknowledge Mahar Mardjono National Brain Center Hospital for supporting this study. The authors also thank Dr. Pratiwi Raissa Windiani and Dr. Kelvin Theandro Gotama for correcting and editing the English manuscript.
Financial Disclosure
No funding was received for this study.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships which could be construed as a potential conflict of interest.
Informed Consent
The ethics committee decided that informed consent for this study was not required, as no personal information of patients was included.
Author Contributions
BTP, BR, and RGK contributed to the conception, design, and acquisition of the study. BR conducted the data analysis and wrote the manuscript. RGK and BTP contributed to the manuscript revision. All authors contributed to reading and approving the submitted version of the manuscript.
Data Availability
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
| References | ▴Top |
- Seibert B, Tummala RP, Chow R, Faridar A, Mousavi SA, Divani AA. Intracranial aneurysms: review of current treatment options and outcomes. Front Neurol. 2011;2:45.
doi pubmed pmc - Sabouri M, Mahabadi A, Tabesh H, Rezvani M, Kouchekzadeh M, Namazi A. Epidemiologic and demographic features, therapeutic intervention and prognosis of the patients with cerebral aneurysm. Adv Biomed Res. 2018;7:6.
doi pubmed pmc - Damiano RJ, Tutino VM, Paliwal N, Patel TR, Waqas M, Levy EI, Davies JM, et al. Aneurysm characteristics, coil packing, and post-coiling hemodynamics affect long-term treatment outcome. J Neurointerv Surg. 2020;12(7):706-713.
doi pubmed pmc - Ries T, Groden C. Endovascular treatment of intracranial aneurysms: long-term stability, risk factors for recurrences, retreatment and follow-up. Klin Neuroradiol. 2009;19(1):62-72.
doi pubmed - Li H, Pan R, Wang H, Rong X, Yin Z, Milgrom DP, Shi X, et al. Clipping versus coiling for ruptured intracranial aneurysms: a systematic review and meta-analysis. Stroke. 2013;44(1):29-37.
doi pubmed - Sadato A, Hayakawa M, Adachi K, Nakahara I, Hirose Y. Large residual volume, not low packing density, is the most influential risk factor for recanalization after coil embolization of cerebral aneurysms. PLoS One. 2016;11(5):e0155062.
doi pubmed pmc - Vanzin JR, Abud DG, Rezende MT, Moret J. Number of coils necessary to treat cerebral aneurysms according to each size group: a study based on a series of 952 embolized aneurysms. Arq Neuropsiquiatr. 2012;70(7):520-523.
doi pubmed - Monsivais D, Morales M, Day A, Kim D, Hoh B, Blackburn S. Cost Analysis of Endovascular Coiling and Surgical Clipping for the Treatment of Ruptured Intracranial Aneurysms. World Neurosurg. 2018.
doi pubmed - https://www.angiocalc.com/.
- Lai HP, Cheng KM, Yu SC, Au Yeung KM, Cheung YL, Chan CM, Poon WS, et al. Size, location, and multiplicity of ruptured intracranial aneurysms in the Hong Kong Chinese population with subarachnoid haemorrhage. Hong Kong Med J. 2009;15(4):262-266.
pubmed - Thien A, See AA, Ang SY, Primalani NK, Lim MJ, Ng YP, King NK. Prevalence of asymptomatic unruptured intracranial aneurysms in a Southeast Asian population. World Neurosurg. 2017;97:326-332.
doi pubmed - Swatan JP, Sani AF, Kurniawan D, Swatan H, Husain S. What are the predictors of intracranial aneurysm rupture in indonesian population based on angiographic findings? Insight from intracranial aneurysm registry on three comprehensive stroke centres in Indonesia. Stroke Res Treat. 2022;2022:4787048.
doi pubmed pmc - Korja M, Kivisaari R, Rezai Jahromi B, Lehto H. Size and location of ruptured intracranial aneurysms: consecutive series of 1993 hospital-admitted patients. J Neurosurg. 2017;127(4):748-753.
doi pubmed - Junior JR, Telles JPM, da Silva SA, Iglesio RF, Brigido MM, Pereira Caldas JGM, Teixeira MJ, et al. Epidemiological analysis of 1404 patients with intracranial aneurysm followed in a single Brazilian institution. Surg Neurol Int. 2019;10:249.
doi pubmed pmc - White JB, Ken CG, Cloft HJ, Kallmes DF. Coils in a nutshell: a review of coil physical properties. AJNR Am J Neuroradiol. 2008;29(7):1242-1246.
doi pubmed pmc - Thaci B, Nuno M, Varshneya K, Gerndt CH, Kercher M, Dahlin BC, Waldau B. Three-dimensional aneurysm volume measurements show no correlation between coil packing density and recurrence. Heliyon. 2020;6(10):e05170.
doi pubmed pmc - Higashida T, Uchida T, Osakabe M, Takahashi Y, Kanazawa R. Efficacy of a 14-coil for framing in coil embolization of small cerebral aneurysms. J Neuroendovasc Ther. 2020;14(9):351-357.
doi pubmed pmc - Ishida W, Sato M, Amano T, Matsumaru Y. The significant impact of framing coils on long-term outcomes in endovascular coiling for intracranial aneurysms: how to select an appropriate framing coil. J Neurosurg. 2016;125(3):705-712.
doi pubmed - Zhang K, Wang ZL, Gao BL, Xue JY, Li TX, Zhao TY, Cai DY, et al. Use of a first large-sized coil versus conventional coils for embolization of cerebral aneurysms: effects on packing density, coil length, and durable occlusion. World Neurosurg. 2019;127:e685-e691.
doi pubmed - Li Y, Zhang M, Verrelli DI, Chong W, Ohta M, Qian Y. Numerical simulation of aneurysmal haemodynamics with calibrated porous-medium models of flow-diverting stents. J Biomech. 2018;80:88-94.
doi pubmed - Giacomini L, Piske RL, Baccin CE, Barroso M, Joaquim AF, Tedeschi H. Neurovascular reconstruction with flow diverter stents for the treatment of 87 intracranial aneurysms: Clinical results. Interv Neuroradiol. 2015;21(3):292-299.
doi pubmed pmc - Kaesmacher J, Muller-Leisse C, Huber T, Boeckh-Behrens T, Haller B, Shiban E, Friedrich B, et al. Volume versus standard coils in the treatment of intracranial aneurysms. J Neurointerv Surg. 2016;8(10):1034-1040.
doi pubmed - Murayama Y, Nien YL, Duckwiler G, Gobin YP, Jahan R, Frazee J, Martin N, et al. Guglielmi detachable coil embolization of cerebral aneurysms: 11 years' experience. J Neurosurg. 2003;98(5):959-966.
doi pubmed - Sluzewski M, van Rooij WJ, Slob MJ, Bescos JO, Slump CH, Wijnalda D. Relation between aneurysm volume, packing, and compaction in 145 cerebral aneurysms treated with coils. Radiology. 2004;231(3):653-658.
doi pubmed - Slob MJ, van Rooij WJ, Sluzewski M. Coil thickness and packing of cerebral aneurysms: a comparative study of two types of coils. AJNR Am J Neuroradiol. 2005;26(4):901-903.
pubmed pmc - Tosello RT, Batista UC, Pereira BJA, Piske RL. Packing density necessary to reach a high complete occlusion rate in circumferential unruptured intracranial aneurysms treated with stent-assisted coil embolization. AJNR Am J Neuroradiol. 2017;38(10):1973-1977.
doi pubmed pmc - Vogler Iv J, Gemender M, Samoilov D. Packing density and long-term occlusion after transcatheter vessel embolization with soft, bare-platinum detachable coils. American Journal of Interventional Radiology. 2020;4:2.
- Piotin M, Spelle L, Mounayer C, Salles-Rezende MT, Giansante-Abud D, Vanzin-Santos R, Moret J. Intracranial aneurysms: treatment with bare platinum coils—aneurysm packing, complex coils, and angiographic recurrence. Radiology. 2007;243(2):500-508.
doi pubmed - Lee JY, Kwon BJ, Cho YD, Kang HS, Han MH. Reappraisal of anatomic outcome scales of coiled intracranial aneurysms in the prediction of recanalization. J Korean Neurosurg Soc. 2013;53(6):342-348.
doi pubmed pmc - Hoh BL, Chi YY, Dermott MA, Lipori PJ, Lewis SB. The effect of coiling versus clipping of ruptured and unruptured cerebral aneurysms on length of stay, hospital cost, hospital reimbursement, and surgeon reimbursement at the university of Florida. Neurosurgery. 2009;64(4):614-619; discussion 619-621.
doi pubmed - Gandhoke GS, Pandya YK, Jadhav AP, Jovin T, Friedlander RM, Smith KJ, Jankowitz BT. Cost of coils for intracranial aneurysms: clinical decision analysis for implementation of a capitation model. J Neurosurg. 2018;128(6):1792-1798.
doi pubmed - Rezek I, Mousan G, Wang Z, Murad MH, Kallmes DF. Coil type does not affect angiographic follow-up outcomes of cerebral aneurysm coiling: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2013;34(9):1769-1773.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
