| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://www.neurores.org |
Case Report
Volume 14, Number 2, September 2024, pages 86-89
Vagal Nerve Stimulation for Intractable Hiccups
Amir Sulimana, c, Menaka Pasangy Paranathalaa, Abdulrahman Kolapob, Uma Nathb, Mohammed Akbar Hussaina
aDepartment of Neurosurgery, Royal Victoria Infirmary, Newcastle, UK
bDepartment of Neurology, Sunderland Royal Hospital, Sunderland, UK
cCorresponding Author: Amir Suliman, Department of Neurosurgery, Royal Victoria Infirmary, Newcastle, UK
Manuscript submitted April 21, 2024, accepted August 23, 2024, published online September 16, 2024
Short title: Vagal Nerve Stimulation for Intractable Hiccups
doi: https://doi.org/10.14740/jnr792
| Abstract | ▴Top |
Intractable hiccups are those lasting beyond a month; they can lead to significant morbidity. We described the case of a patient with intractable hiccups after intracranial surgery, which was refractory to multiple pharmacological agents. Eventually, insertion of vagal nerve stimulator led to resolution of the hiccups. A number of cases have been described of the utility of vagal nerve stimulation in treating intractable hiccups. Here we outlined the indications as well as hypothesized mechanism of action. We proposed this treatment to be considered in the most refractory cases.
Keywords: Epilepsy; Hiccups; Intractable; Singultus; Vagal nerve stimulation; Vagus nerve
| Introduction | ▴Top |
Hiccup, or singultus, is a sudden onset of abnormal erratic involuntary spasmodic contraction of the diaphragmatic and intercostal muscle of the diaphragm, followed by a sudden closure of the glottis, which is often repetitive in nature [1]. Hiccups are predominantly benign, of short duration and often resolve spontaneously. Hiccups that last more than 48 h are termed persistent, and if longer than a month are termed intractable [2]. When hiccups become prolonged or intractable, they can interrupt eating, talking and even sleep. As a result, they can thus lead to dehydration, severe malnutrition, and weight loss. They can worsen pain, cause psychological stress, mood changes and fatigue, adversely impacting quality of life [1, 2]. In patients with persistent or intractable hiccups, a cause is often not found.
Most hiccups lasting more than 48 h require treatment with medication unless a reversible cause is identified. There are a number of pharmacological agents which have been used, with most related to the gamma-aminobutyric acid (GABA) and dopaminergic pathway [1]. There is no clear evidence for which is most efficacious [1]. If an underlying etiology is found, the appropriate medication should be initiated, such as proton pump inhibitors for duodenal ulcer or gastroesophageal reflux. Baclofen, a GABA agonist, is particularly useful for central causes. Along with gabapentin, it is considered a first-line option for intractable hiccups of unclear etiology. Their efficacy has been shown when compared against placebo in a randomized controlled trial [3]. Side effects can however be an issue. Metoclopramide and chlorpromazine can also be used [1]; the latter has the advantage of being able to be administered parenterally. Combining medications can be a useful technique. A variety of other medications have been used including pregabalin, amitriptyline, sertraline, haloperidol, phenytoin, and valproic acid [2]. Even high-dose benzodiazepines have been used in an effort to control very troublesome hiccups [1]. When hiccups are not controlled despite use of pharmacotherapy, alternative medical treatment such has hypnosis, acupuncture and psychotherapy have been considered although benefits remain uncertain [4]. Alongside pharmacological methods of management, vagal nerve maneuvers such as vomiting or ocular pressure are used in termination of hiccups [5]. This has led to interest in stimulation of the nerve as a therapy option.
| Case Report | ▴Top |
We present a 64-year-old male with previous medical history of ulcerative colitis and epilepsy due to right hippocampal sclerosis. He underwent magnetic resonance imaging (MRI) for investigation of seizures, which showed a fourth ventricle lesion for which he underwent midline posterior fossa craniotomy and excision of the lesion in June 2018 (Fig. 1). This was found on histological examination to be a sub ependymoma (World Health Organization (WHO) grade I). Postoperatively, he suffered from significant problems with nausea, vomiting and hiccups. The nausea and vomiting settled with antiemetics; however, his hiccups persisted beyond 1 month and became intractable.
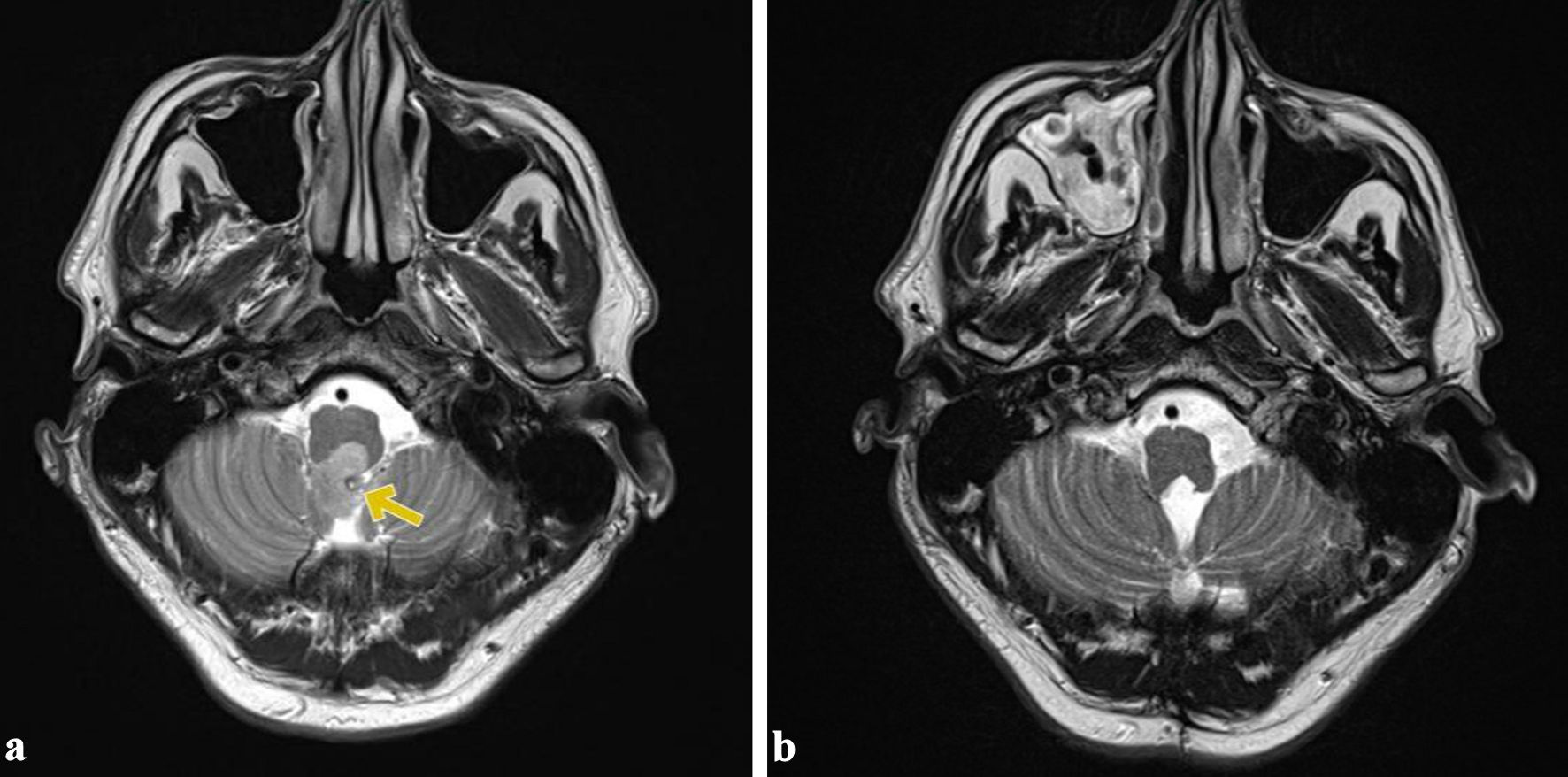 Click for large image | Figure 1. Preoperative and postoperative appearances. (a) The fourth ventricle lesion (yellow arrow). (b) Postoperative image showing total resection of the lesion. |
He was significantly troubled by the hiccups which occurred up to 10 times a day. He had no history of loss of awareness with the hiccups, and they were his main disabling symptoms as they were impacting his swallowing and affecting every aspect of his daily life. He was started on gabapentin and baclofen with some initial improvement, but hiccups persisted. He was started on a short course of chlorpromazine, but this did not help, and he did not tolerate the side effects. Subsequently, he was started on oral metoclopramide.
Given the lack of improvement, he was admitted and investigated. His neurological examination was normal. He had an MRI of the brain which showed no recurrence of the excised lesion. Computed tomography (CT) scan of the chest, abdomen and pelvis identified no intraabdominal cause for his hiccups. Blood investigations results showed no biochemical abnormalities that would cause hiccups. He had an electroencephalogram performed, which showed no abnormalities, as his seizures had been well controlled since before his surgery. He had medications dosages increased and had a trial of intravenous metoclopramide via syringe driver, which he did not tolerate. He was subsequently also trialed on amitriptyline starting at 10 mg nightly and slowly titrated up to 50 mg. He was also started on clonazepam. He was reviewed by the neurology, ENT (ear, nose, and throat) and speech and language therapy specialties and tried a variety of treatments, all of which were unsuccessful in controlling his intractable hiccups.
After a review by the neurosurgical team, the option of vagus nerve stimulation was discussed with the patient based on the limited risk involved and the degree to which the symptoms were affecting his life. An additional benefit of this was to aid seizure management. After obtaining informed consent, he underwent implantation of a left vagal nerve stimulator in December 2020. The operation was uneventful, and he had a satisfactory postoperative recovery.
The initial stimulator settings were output current at 0.25 mA and magnet stimulation at 0.5 mA. On clinic review of 2 weeks after the operation, he had noticeable improvement of his symptoms, with reduction of the frequency of the hiccups to once every few days, reduction of choking episodes and better coordination of swallowing. The pharmacological treatment for the hiccups was discontinued. The settings of the stimulator were changed as the output current increased to 0.375 mA, and the magnet stimulation was reduced to 0.375 mA. He has complete resolution of the hiccups, and the swallowing difficulties after the setting has been changed without any significant side effects from the vagal nerve stimulation. Therefore, it was concluded that the vagal nerve stimulator has been successful in treating his hiccups, given the improvement with the hiccups control after the increase of the vagal nerve stimulator settings, and hence the stimulator has not been turned off since insertion. He was reviewed after 4 weeks and then after 6 months and continued to have annual follow-ups till date. He has had no recurrence of hiccups till date.
| Discussion | ▴Top |
The pathophysiology of hiccups remains unclear, but it is thought to be a reflex response [1, 6] with several neural pathways being involved. Figure 2 depicts the anatomy and the related pathways of the hiccups reflex arc. The afferent limb of the reflex arc includes the phrenic nerve, the vagus nerve and the sympathetic chain (T6 - T12). The central nervous system (CNS) mediators involved in the hiccup response are believed to be the medulla oblongata and the spinal cord segments C3 - C5, with possible modulation from hypothalamus, midbrain, reticular activating system, the respiratory center, globus pallidus, subthalamic nucleus, temporal lobes and nuclei of phrenic nerves [6, 7]. The efferent limb in hiccups has been attributed to the phrenic nerve to the diaphragm. Accessory efferent nerves to the glottis and intercostal muscles are also efferent of this arc. If any part of this reflex arc is affected, it can trigger bouts of hiccups. The CNS and the gastrointestinal tract appear to be the most common culprits [8]; however, irritation of the phrenic nerve anywhere along its course is associated with hiccups. Irritation of the vagus nerve and branches may also be a precipitant of hiccups [9-11]. Studies have suggested this to be the mechanism associated with hiccups occurring in the postoperative period [2]. Medications, toxic metabolic states, as well as psychogenic factors have all been identified as causes of prolonged hiccups [2]. Pharmacological interventions are likely to act at various sites at this reflex arc.
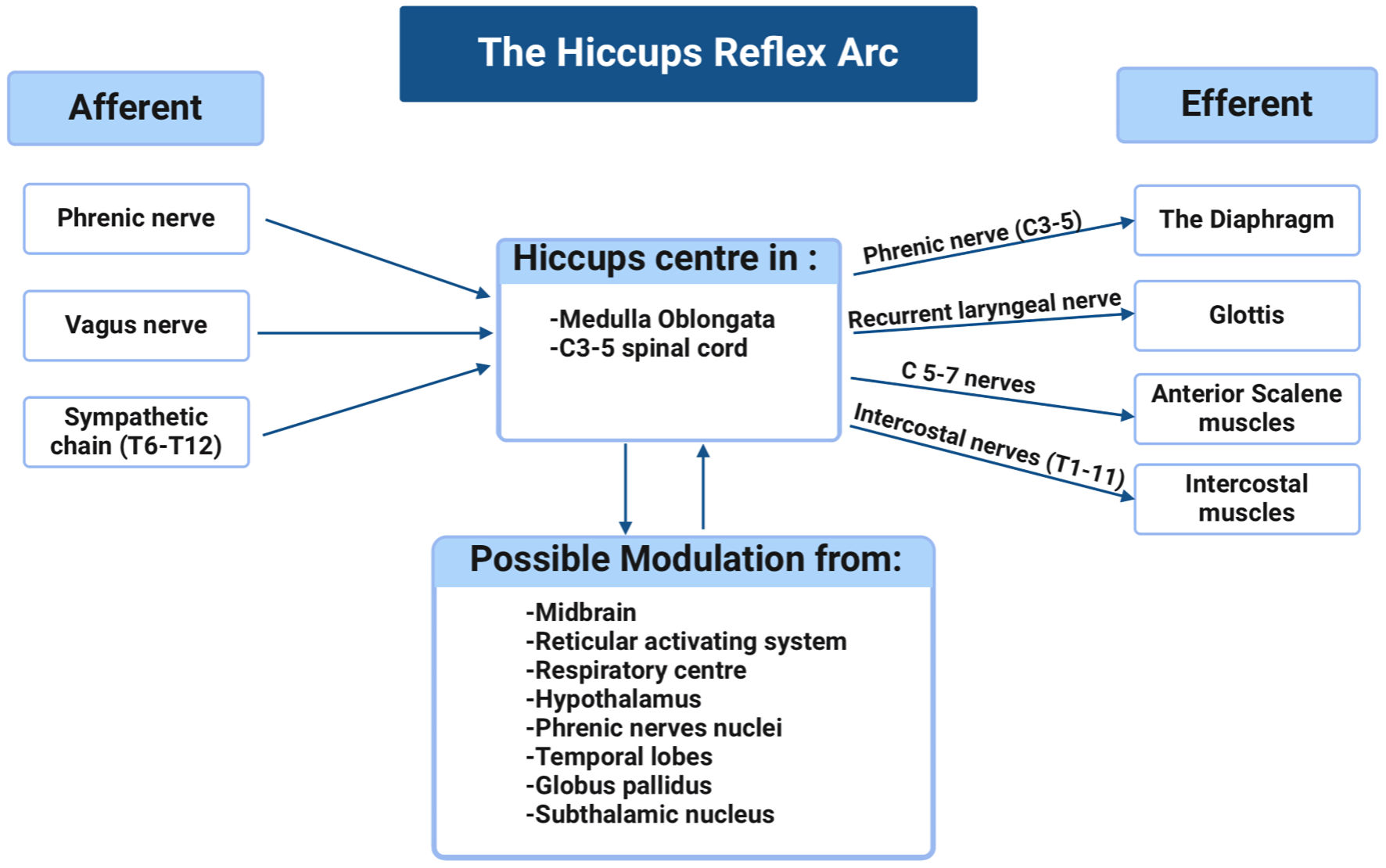 Click for large image | Figure 2. The anatomy and the related pathways of the hiccups reflex arc. |
The role of vagal nerve stimulation in affecting hiccups is not yet fully understood. Since the first reported case of the management of intractable hiccup using vagus nerve stimulation by Payne et al [12] in 2005, there have been a total of six cases [12-17], except ours, in the literature. The youngest patient was 47, and the oldest was 85 years old; and 85% of patients were male. In four patients (57%), the cause of hiccups was intracranial pathology. Chest infection was the cause in another patient. Six cases were managed with vagus nerve stimulator, and one case underwent transcutaneous nerve stimulator. Five cases (71%) have complete relief after VNS insertion, one case has partial improvement, and one has no improvement [13]. The cases are presented in Table 1 [12-17]. The mechanism by which vagal nerve stimulation ameliorates hiccups is not fully understood. It may be postulated based on the proposed reflex arc underpinning development of hiccups. The stimulation of the vagal nerve may be regulating the central nervous mediation of hiccups and disrupting the reflex arc. Interestingly, it has been recently reported that a patient developed intractable hiccups after insertion of vagal nerve stimulator, which suggests the influence of vagal nerve stimulation on the hiccups reflex arc [18]. The side effects of vagal nerve stimulation are minimal, and the risks of the procedure are similar to those of any other surgery, including infection, bleeding, and those of general anesthesia [19]. Specific risks include damage to local structures such as the carotid artery and the jugular vein in the carotid sheath or failure of the procedure to provide any benefit.
 Click to view | Table 1. Existing Cases of Vagal Nerve Stimulation of Treatment of Intractable Hiccups |
Conclusions
Intractable hiccups cause notable morbidity and have a significant impact on quality of life. In our case and previously reported cases, vagal nerve stimulator is an effective treatment for intractable hiccups, with minimal risk and side effects. We suggest it should be considered for cases refractory to medical management.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
Informed consent was obtained.
Author Contributions
Amir Suliman: main author, neurology and neurosurgery literature review, communication with the patient and the team. Menaka Pasangy Paranathala: neurosurgery literature review. Abdulrahman Kolapo: neurology literature review. Uma Nath: the patient’s primary neurologist and paper reviewer. Mohammed Akbar Hussain: the patient’s primary neurosurgeon and paper reviewer.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Jeon YS, Kearney AM, Baker PG. Management of hiccups in palliative care patients. BMJ Support Palliat Care. 2018;8(1):1-6.
doi pubmed - Marinella MA. Diagnosis and management of hiccups in the patient with advanced cancer. J Support Oncol. 2009;7(4):122-127, 130.
pubmed - Zhang C, Zhang R, Zhang S, Xu M, Zhang S. Baclofen for stroke patients with persistent hiccups: a randomized, double-blind, placebo-controlled trial. Trials. 2014;15:295.
doi pubmed pmc - Moretto EN, Wee B, Wiffen PJ, Murchison AG. Interventions for treating persistent and intractable hiccups in adults. Cochrane Database Syst Rev. 2013;2013(1):CD008768.
doi pubmed pmc - Petroianu GA. Treatment of hiccup by vagal maneuvers. J Hist Neurosci. 2015;24(2):123-136.
doi pubmed - Howes D. Hiccups: a new explanation for the mysterious reflex. Bioessays. 2012;34(6):451-453.
doi pubmed pmc - Sweeney J, Bodman A, Hall WA. Brain Abscess of Basal Ganglia Presenting with Persistent Hiccups. World Neurosurg. 2018;112:182-185.
doi pubmed - Strate T, Langwieler TE, Mann O, Knoefel WT, Izbicki JR. Intractable hiccup: an odd complication after laparoscopic fundoplication for gastroesophageal reflux disease. Surg Endosc. 2002;16(7):1109.
doi pubmed - Appenzeller O. The autonomic nervous system and fatigue. Funct Neurol. 1987;2(4):473-485.
pubmed - Clancy JA, Deuchars SA, Deuchars J. The wonders of the Wanderer. Exp Physiol. 2013;98(1):38-45.
doi pubmed - Cunningham ET, Jr., Ravich WJ, Jones B, Donner MW. Vagal reflexes referred from the upper aerodigestive tract: an infrequently recognized cause of common cardiorespiratory responses. Ann Intern Med. 1992;116(7):575-582.
doi pubmed - Payne BR, Tiel RL, Payne MS, Fisch B. Vagus nerve stimulation for chronic intractable hiccups. Case report. J Neurosurg. 2005;102(5):935-937.
doi pubmed - Grewal SS, Adams AC, Van Gompel JJ. Vagal nerve stimulation for intractable hiccups is not a panacea: a case report and review of the literature. Int J Neurosci. 2018;128(12):1114-1117.
doi pubmed - Longatti P, Basaldella L, Moro M, Ciccarino P, Franzini A. Refractory central supratentorial hiccup partially relieved with vagus nerve stimulation. J Neurol Neurosurg Psychiatry. 2010;81(7):821-822.
doi pubmed - Schulz-Stubner S, Kehl F. Treatment of persistent hiccups with transcutaneous phrenic and vagal nerve stimulation. Intensive Care Med. 2011;37(6):1048-1049.
doi pubmed - Tariq K, Das JM, Monaghan S, Miserocchi A, McEvoy A. A case report of Vagus nerve stimulation for intractable hiccups. Int J Surg Case Rep. 2021;78:219-222.
doi pubmed pmc - De Vloo P, Dallapiazza RF, Lee DJ, Zurowski M, Peng PW, Chen R, Hodaie M. Long-term relief of intractable hiccups with vagal nerve stimulation. Brain Stimul. 2018;11(6):1385-1387.
doi pubmed - Recio SZ, Abdennadher M. Intractable hiccups after VNS implantation: a case report. BMC Neurol. 2023;23(1):297.
doi pubmed pmc - Penry JK, Dean JC. Prevention of intractable partial seizures by intermittent vagal stimulation in humans: preliminary results. Epilepsia. 1990;31 Suppl 2:S40-43.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
