| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://www.neurores.org |
Original Article
Volume 14, Number 2, December 2024, pages 74-85
Demographics and Clinical Correlates of Blood Pressure Among Ugandans at Risk for Stroke
Martha Sajatovica, b, c, Martin Kaddumukasad, Josephine Nambi Najjumae, Scovia Nalugo Mbalindaf, Jane Nakibuukad, Doreen Birungij, Carla Conroyb, c, Joy Yalab, c, Levicatus Mugenyig, Christopher J. Buranth, i, Shirley Moorei, Elly T. Katabiraj, Mark Kaddumukasaj, k
aNeurological and Behavioral Outcomes Center, University Hospitals Cleveland Medical Center, Cleveland, OH 44106, USA
bDepartment of Medicine, University Hospitals Cleveland Medical Center, Cleveland, OH 44106, USA
cSchool of Medicine, Case Western Reserve University, Cleveland, OH, USA
dDepartment of Medicine, Mulago Hospital, Kampala, Uganda
eDepartment of Nursing, Mbarara University of Science and Technology, Mbarara, Uganda
fDepartment of Nursing, College of Health Sciences, Makerere University, Kampala, Uganda
gCollege of Health Sciences, Makerere University, Kampala, Uganda
hLouis Stokes VA Medical Center, Geriatric Research Education, and Clinical Center, Cleveland, OH 44106, USA
iFrances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, OH, USA
jDepartment of Medicine, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda
kCorresponding Author: Mark Kaddumukasa, Department of Medicine, School of Medicine, College of Health Sciences, Makerere University, Kampala, Uganda
Manuscript submitted July 10, 2024, accepted October 18, 2024, published online November 15, 2024
Short title: Correlates of BP and Risk for Stroke
doi: https://doi.org/10.14740/jnr830
| Abstract | ▴Top |
Background: Stroke risk factors are an emerging public health problem in Sub-Saharan Africa. This analysis examined demographic and clinical correlates of blood pressure (BP) in a Ugandan sample at risk for stroke.
Methods: We conducted a cross-sectional analysis of demographics, stroke risk factors, and selected clinical variables associated with systolic blood pressure (SBP) and diastolic blood pressure (DBP). Demographics (age, gender, marital status, education level, rural/suburban/urban status, and employment status), stroke risk factors (diabetes, hyperlipidemia, obesity, smoking status, sedentary lifestyle, and problem alcohol use), and clinical variables associated with SBP and DBP were derived from the screening and baseline sample of a prospective, randomized effectiveness-implementation trial testing a novel stroke risk reduction approach (TargetEd manAgeMent Intervention (TEAM)) conducted across three Ugandan sites. We examined variables with respect to an established set of guidelines for hypertension (HTN) severity, the European Society of Cardiology and the European Society of Hypertension (ESC-ESH) Guideline.
Results: Of the total sample of 247, the mean sample age was 55.4 years (standard deviation (SD) = 12.0), with a female predominance (n = 168, 68%). In addition to HTN, the most common sample stroke risk factors were hyperlipidemia (n = 199, 80.6%) and obesity (n = 98, 39.7%). The majority (n = 238, 96.4%) were prescribed at least one medication to treat HTN. Mean SBP and DBP at baseline were 143.0 (SD = 19.8, range 94.5 - 206) and 89.3 (SD = 14.0, range 61 - 136), respectively. ESC-ESH classifications were grouped into grades of increasing severity from the mildest (grade 1) to the most severe (grade 3). An additional < grade 1 was created to reflect individuals whose ESC-ESH scores dropped below grade 1 post-screening. There were few significant differences across ESC-ESH groups, except that having diabetes, being sedentary, and being a smoker were associated with higher ESC-ESH grades.
Conclusions: To help reduce the stroke burden in Uganda, our findings support the importance of raising awareness of HTN and helping individuals to manage their HTN with both medications and lifestyle approaches.
Keywords: Stroke; Modifiable risk factors; Hypertension; Sub-Saharan Africa
| Introduction | ▴Top |
Neurological conditions such as stroke contribute substantially to burden or disability [1] and cause 16.8% of deaths in lower- and middle-income countries (LMICs) compared with 13.2% of deaths in high-income countries [1, 2]. Unfortunately, stroke risk factors, which were once rare in traditional African societies, are an emerging public health problem [3]. A growing number of individuals with a sedentary lifestyle, tobacco and alcohol use, and/or high fat/salt/cholesterol diets, all increase population stroke risk [4]. In addition, population aging and urban migration are associated with the stroke risk factors of obesity and diabetes. Taken together, it is perhaps not surprising that in Sub-Saharan Africa (SSA), stroke occurs at relatively early ages, resulting in a substantial cumulative burden [4, 5].
While data projections are sobering, an important point to consider in reducing stroke burden in LMICs is that many stroke risk factors such as hypertension (HTN), obesity, diabetes, tobacco use, sedentary lifestyle, high fat/high salt diet, and smoking are potentially modifiable. Reducing stroke risk factors may be particularly highly effective in reducing stroke. For example, while every 20/10 mm Hg increase in blood pressure (BP) doubles the mortality from stroke, the use of antihypertensive therapy can reduce stroke risk by 35-40% [6, 7]. In Western Uganda, HTN has been reported in 30.5% of adults over the age of 20 years [8]. Thus, HTN is a key actionable target for stroke risk reduction in SSA and targeting individuals with poorly controlled BP may help reduce individual- and population-level risk.
In spite of the critical need to manage stroke risk in Uganda and SSA more broadly, the literature on effective approaches to manage HTN and other stroke risk factors in these settings is limited [9, 10]. This data analysis, derived from a baseline sample enrolled in an ongoing US National Institute of Neurological Disorders and Stroke (NINDS)-funded randomized controlled trial, examined demographics, stroke risk factors, and clinical correlates of BP in a Ugandan sample at risk for stroke. A deeper understanding of correlates of poorly controlled BP could potentially inform care approaches that target individuals and communities at risk.
| Materials and Methods | ▴Top |
Overview
The parent study, from which these data were derived, is a prospective, randomized effectiveness-implementation trial of two stroke reduction approaches (TargetEd manAgeMent Intervention (TEAM) vs. Enhanced Treatment as Usual (ETAU)) in 247 Ugandans at risk for stroke. Details of the study protocol have been published elsewhere [11]. The project is being conducted across three Ugandan sites enrolling a representative sample of Ugandans at risk for stroke. For this analysis, only study screening and baseline data were used, and we conducted a cross-sectional analysis of demographics, stroke risk factors, and selected clinical variables associated with systolic blood pressure (SBP) and diastolic blood pressure (DBP). The screening process for stroke risk factors was based upon an initial self-reported assessment of having or not having diabetes, hyperlipidemia, obesity, smoking, problem alcohol use or sedentary lifestyle as well as an initial single screening BP measurement. To complete calculation of a screening BP, the BP measurement was repeated after 3 days to confirm the high SBP taking into account possible white coat HTN, and/or optimizing the drugs prescribed for cardiovascular risk reduction. Based on the second BP measurement (post initial screening BP evaluation), those found with high SBP and confirmed to have two or more stroke risk factors based on laboratory testing were considered “enrolled” and then completed study baseline evaluation.
This study was approved by the School of Medicine, Research and Ethics Committee (SOMREC) Mak-SOMREC-2023-648 and UNCST HS2944ES. All experiments were performed in accordance with the relevant guidelines and regulations (Declaration of Helsinki).
Sample
All individuals were 18 years of age or older and were deemed to be at risk for stroke based upon the following: 1) High SBP defined as ≥ 140 mm Hg assessed on at least two occasions at least 3 days apart and either criterion 2 or 3 as noted below: 2) At least one other modifiable stroke risk factor including diabetes, hyperlipidemia, obesity, smoking, problem alcohol use or sedentary lifestyle; 3) History of stroke or transient ischemic attack (TIA) within the past 5 years.
All study participants provided informed consent for participation. All study participants with normal BP at screening were excluded. The enrolled sample was selected to be as broadly generalizable as possible to the general population of Ugandans at risk for stroke and there were minimal exclusion criteria. Based on our study inclusion criteria, we enrolled subjects who had a high SBP and at least one other modifiable stroke risk factor at screening. While medication treatments for HTN are effective in lowering BP, individuals can still have suboptimal BP control for a variety of reasons including poor adherence, medication dosing being suboptimal, or being on a medication that is not ideal for that individual. The stroke risk reduction intervention that is being tested in the overall randomized controlled trial is intended to help individuals better manage their BP and general cardiovascular risk by making appropriate lifestyle changes and/or communicating with healthcare providers to identify treatments to help them achieve optimal BP control. Individuals who had dementia, those with sickle-cell disease, those who were pregnant or those who were unable to participate in study procedures were excluded from participation.
Variables
This baseline sample analysis examined demographics (age, gender, marital status, educational level, rural/suburban/urban status, and employment status) and selected clinical variables in relation to baseline HTN components including SBP, DBP and consideration with respect to an established set of guidelines for HTN severity.
HTN variables
SBP and DBP
All BP assessments used a standardized protocol in a medical outpatient clinic at the various hospitals. Prior to BP measurement, study participants were requested beforehand to refrain from smoking and drinking alcohol or caffeinated beverages at least half an hour before the examination. BP was measured with an Omron automated sphygmomanometer model HEM 907 whose accuracy has been validated [12]. The participant was asked to sit on a chair and rest quietly for 15 min with his/her legs uncrossed. The left arm was then placed on a table with the palm facing upward and the ante-cubital fossa at the level of the lower sternum. Three measurements were taken at least 5 min apart. The average of the last two readings were considered to be the final BP reading.
HTN classification
All sample participants had elevated SBP at study screening defined as SBP of 140 or higher. Levels of HTN severity were classified post hoc using the European Society of Cardiology and the European Society of Hypertension (ESC-ESH) Guideline published in 2018 [13]. The ESC-ESH classifications are organized into grades of increasing severity with grade 1 being the mildest category and grade 3 being the most severe. Grade 1 is defined as SBP 140 - 159 mm Hg and/or DBP 90 - 99 mm Hg. Grade 2 is defined as SBP 160 - 179 mm Hg and/or DBP 100 - 109 mm Hg. Grade 3 is defined as SBP ≥ 180 mm Hg and/or DBP ≥ 110 mm Hg. For analyses, a fourth ESC-ESH grade was created to reflect SBP < 140 mm Hg and DBP < 90 mm Hg. In addition to SBP, DBP and ESC-ESH classification, we also assessed whether an individual was prescribed medication to manage HTN.
Other stroke risk factors
Diabetes
Diabetes was defined as having a glycosylated hemoglobin (HbA1c) level of ≥ 6.5%.
Hyperlipidemia
Hyperlipidemia was defined as having abnormal/elevated serum cholesterol/lipids. The serum assessments conducted included cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), and triglycerides. Normal reference ranges for cholesterol were 0 - 5.17 mmol/L, for LDL were 0 - 4.11 mmol/L, for HDL were 1.15 - 3.3 mmol/L, and for triglycerides were 0 - 2.3 mmol/L. For this analysis, elevated cholesterol was defined as > 5.2 mmol/L, elevated LDL was defined as > 3.4 mmol/L, and elevated triglycerides were defined as > 1.7 mmol/L. For HDL, abnormal values of concern were lower than the reference range and differed for men and women. Abnormal HDL was defined as < 1.0 mmol/L for men and < 1.3 mmol/L for women.
Obesity
Obesity was classified using body mass index (BMI) with a value of > 30 classified as obese.
Smoking status
Tobacco use was measured by the Global Adult Tobacco Survey (GATS) questionnaire [14]. Given the very low rates of tobacco use in this sample, smoking status based on the GATS was dichotomized as yes/no.
Problem alcohol use
Problem alcohol use for study screening purposes was assessed with questions on frequency, type of alcohol, and quantity consumed. Participants were classified as engaging in potential problem alcohol use if they exceeded the recommended level for safe alcohol intake, i.e., more than three drinks on average every time they drink, or if they undertook binge drinking (i.e., more than three drinks on one occasion in the 1 month preceding the evaluation) [15, 16]. Alcohol use was also assessed with the Alcohol Use Disorders Identification Test (AUDIT) [17]. The total score on the AUDIT ranges from 0 to 40 with higher scores indicating more severe problems with alcohol. A total score of less than 8 indicates no harmful drinking behavior or alcohol dependence, while a total score of 8 or more indicates harmful drinking behavior. A score of 13 or more in women is likely to indicate alcohol dependence, while a score of 15 or more in men is likely to indicate alcohol dependence. Given the low rates of alcohol use in this sample, any score above 8 was collapsed into a category of harmful drinking behaviors.
Sedentary lifestyle
Screening for sedentary lifestyle used a single question adapted from the Global Physical Activity Questionnaire (GPAQ) [18]. Individuals were classified as having sedentary lifestyle if they answered “yes” to the following question: In a typical week, do you spend at least 150 min doing moderate-intensity activities that cause small increases in breathing and heart rate at work, traveling to places or activities for leisure? Examples of activities are brisk walking/jogging/biking/gardening/housework.
Personal stroke or TIA history
Past stroke or TIA occurrence (within the past 5 years) was assessed at study screening. We also assessed for self-reported family stroke history. Personal and family stroke history were classified into separate dichotomous variables (yes/no).
Data analysis
Univariate descriptive analysis using frequencies and percentages for categorical variables and means, standard deviations (SDs), and ranges for continuous variables is shown in Table 1. Comparisons of baseline demographics and clinical characteristics across the four ESC-ESH cut-points were conducted using Chi-square tests for categorical variables such as gender and education and one-way analysis of variance for continuous. Bonferroni post-hoc tests were used for pairwise group comparisons. Additionally, correlations were used to identify the associations of baseline demographics and clinical characteristics with SBP, DBP, and ESC-ESH HTN severity grade. The HDL values for two extreme outlier cases (due to a presumed genetic variant) were not included in means and correlational analysis for this biomarker. The level of significance for all P-values in this study was set at α ≤ 0.05.
 Click to view | Table 1. Baseline Demographics and Clinical Characteristics of the TEAM Uganda Sample (N = 247 Randomized Sample) |
| Results | ▴Top |
Overall sample
Table 1 shows the demographics and clinical variables of the randomized baseline sample. Mean age was 55.4 (SD = 12.0), with a range of 20 - 90 years. The majority of the sample were female (n = 168, 68%) and nearly half of the sample (n = 118, 47.8%) had a primary-level education. There were 49 individuals (19.8%) who had a previous stroke or TIA and 50 individuals (20.2%) had a family history of stroke. In addition to HTN, the most common stroke risk factors in the screening sample were hyperlipidemia (n = 199, 80.6%) and obesity (n = 98, 39.7%). A scant minority (n = 4, 1.6%) were smokers as identified by the GATS.
Figure 1a and b shows the distribution of SBP and DBP at screening. Figure 2a and b shows the distribution of SBP and DPB at baseline. Notably, the overwhelming majority of the total sample (n = 242, 98%) were prescribed at least one medication to treat stroke/cardiovascular risk prior to their enrollment in the study. As noted in Table 1, of participants prescribed at least one medication, individuals were taking an average of three medications. Participants were prescribed medications in the following categories: calcium channel blockers (N = 204, 84.29%), angiotensin converting enzyme (ACE)/angiotensin II receptor blocker (ARB) drugs (N = 177, 73.14%), alpha- and beta-blockers (N = 98, 40.50%), antiplatelet (N = 67, 27.69%), oral diabetes drugs (N = 48, 21.52%), lipid lowering drugs (N = 50, 20.66%), diuretics (N = 47, 19.43%), insulin (N = 24, 10.71%), combination drugs (N = 4, 1.65%), and anticoagulants (N = 2, 0.83%). Individuals with a personal stroke history were on an average of 3.2 (1.0) medications, while those without a personal stroke history an average of 2.9 (1.3) medications (data not shown).
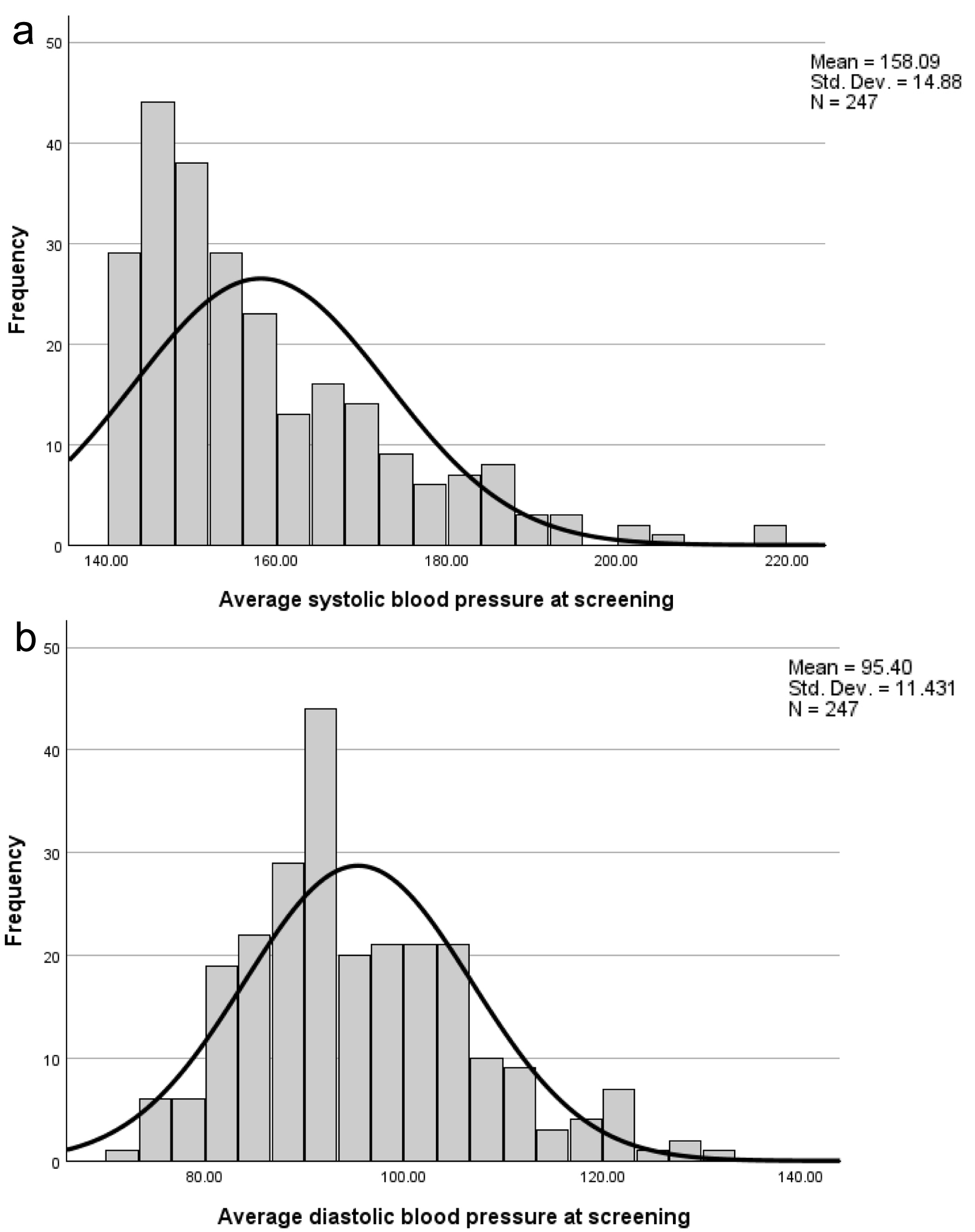 Click for large image | Figure 1. Distribution of SBPs (a) and DPBs (b) in a Ugandan screening sample. SBP: systolic blood pressure; DBP: diastolic blood pressure. |
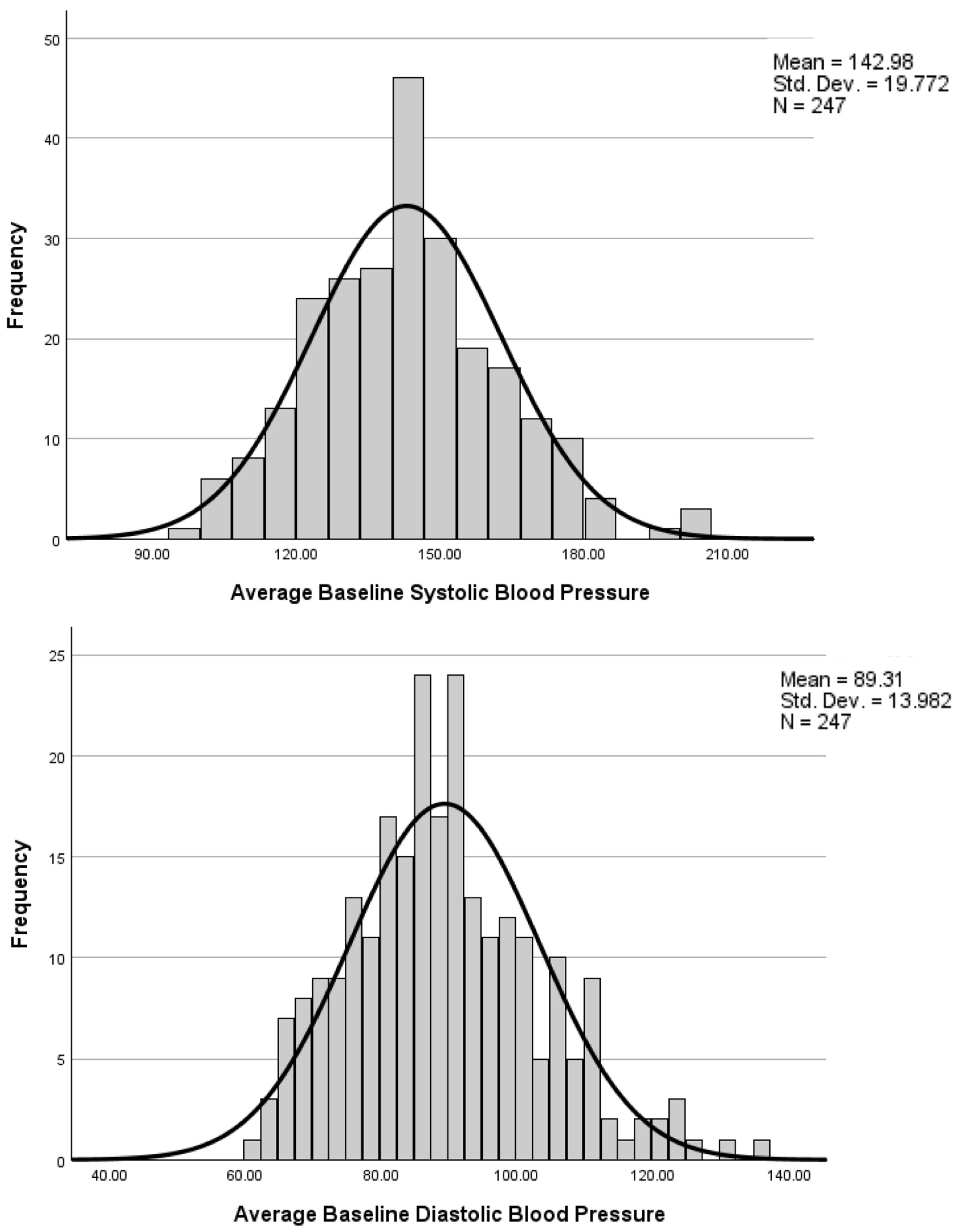 Click for large image | Figure 2. Distribution of SBPs (a) and DBPs (b) in a Ugandan baseline sample. SBP: systolic blood pressure; DBP: diastolic blood pressure. |
While all individuals had HTN and at least one other stroke risk factor at study screening, not all individuals had HTN classified within the ESC-ESH categories by the time they completed study baseline, presumably because individuals had improved adherence with taking medication to manage their BP once they had provided consent to participate in the study.
ESC-ESH HTN grade comparisons with demographics and clinical variables
ESC-ESH classifications were grouped into grades of increasing severity with grade 1 being the least severe and grade 3 being the most severe. An additional classification < grade 1 was created to reflect individuals whose ESC-ESH scores dropped below grade 1 that was identified during screening. The majority of individuals fell into the < grade 1 category (N = 93, 37.7%) or grade 1 category (N = 83, 33.6%) at baseline, while smaller proportions fell into the grade 2 (N = 47, 19%) and grade 3 (N = 24, 9.7%) categories. With respect to correlates of HTN grade, age was not significant; however, Bonferroni comparisons identified that individuals were significantly older in the < grade 1 and grade 1 as compared to the grade 3 group. Significant differences were identified in individuals with a personal history of stroke (Chi-square = 12.35, df = 3, P = 0.006) who had a higher percentage of individuals in < grade 1 as compared to grade 2. Significant differences were identified in individuals with diabetes (Chi-square = 11.29, df = 3, P = 0.01) with a higher percentage of individuals in grades 2 and 3 as compared to < grade 1. Significant differences were identified in individuals with a sedentary lifestyle (Chi-square = 8.11, df = 3, P = 0.04); however, no significant Bonferroni pairwise comparisons were found. Significant differences were identified in individuals with SBP (Welch F = 165.01, df = 3, 76.16, P < 0.001) and DBP (F = 207.80, df = 3,243, P < 0.001). Tamhane T2 for SBP and Bonferroni for DBP pairwise comparisons were significantly different among all groups with higher ESC-ESH grade classifications reflecting higher scores of SBP and DBP. Significant differences were identified for serum LDL (Welch F = 3.26, df = 3, 81.03, P = 0.026). Tamhane T2 comparisons identified that individuals had significantly higher serum LDL levels in the < grade 1 as compared to the grade 2 group. Significant differences were identified in current smokers (Chi-square = 7.83, df = 3, P = 0.05); however, no significant Bonferroni pairwise comparisons were found (Table 2).
 Click to view | Table 2. Comparison of Baseline Demographics and Clinical Characteristics of the TEAM Uganda Sample Classified Using ESC-ESH Cut-Points |
Overall, there were few significant differences across ESC-ESH groups, except that having diabetes, being sedentary, and being a smoker were associated with higher ESC-ESH grades. Somewhat counterintuitively, having a personal stroke history was seen significantly more often in the group with baseline HTN that was below any ESC-ESH grade (SPB < 140 and DPB < 90).
Correlates of HTN severity categories
Table 3 illustrates the associations between demographics and clinical variables, SBP, DBP and any ESC-ESH grade. Factors that were significantly associated with elevated SBP were elevated DBP, having diabetes, having a higher ESC-ESH grade of HTN, being on more stroke/cardiovascular risk reduction medications, and having problem alcohol use. Unexpectedly, being married, and not having a personal stroke/TIA history were also associated with higher SBP. Factors that were significantly associated with higher DBP were older age, higher SBP, having a higher ESC-ESH grade, and having problem alcohol use. As with SBP and unexpectedly, being married, and not having a personal stroke/TIA history were also associated with higher DBP. Similarly, factors that were significantly associated with a higher ESC-ESH grade were elevated SBP and DBP, having diabetes, and having problem alcohol use.
 Click to view | Table 3. Pearson Correlations for Baseline Demographics and Clinical Characteristics of the TEAM Uganda Sample (N = 247) |
| Discussion | ▴Top |
This analysis of screening and baseline data from an ongoing Ugandan clinical trial testing a novel stroke risk reduction approach evaluated demographics and clinical factors associated with BP and HTN. This research sample is at high risk for either first time or recurrent stroke based upon their having multiple stroke risk factors including HTN. Findings have several important clinical/policy and research implications.
The stroke risk factor of HTN has been demonstrated to be both common and incompletely treated in Uganda. A 2009 Ugandan study by Wamala and colleagues estimated that 28.9% of urban adults and 25.8% of rural adults have HTN, with an increase from 14% to 18% in 2005 [8]. A recent retrospective medical record review by Majumdar and colleagues [19] which evaluated nearly 18,000 Uganda adults found an age-standardized prevalence of HTN of 33.4%. In the same report by Majumdar et al [19], older patients had higher rates of HTN vs. younger patients (79% in 66+, as compared to 23% in those aged 18 - 30), as did males (46%) vs. females (38%). A multiple logistic regression analysis describing HTN prevalence and its correlates found older age (odds ratio (OR): 1.06, 95% confidence interval (CI): 1.05 - 1.06, P < 0.001), male gender (OR: 1.15, 95% CI: 1.04 - 1.28, P = 0.007), number of healthcare visits (OR: 1.13, 95% CI: 1.11 - 1.14, P < 0.001), and insurance status (OR: 1.21, 95% CI: 1.05 - 1.39, P = 0.007) to be associated with increased likelihood of HTN [19]. Among those with HTN in the study by Majumdar et al, rates of treatment with antihypertensive medication (39.4%) and BP control (20% overall) were described [19]. This is significantly less than in high-resource settings such as the USA or countries in the Organization for Economic Co-operation and Development (OECD) group [20, 21]. Our findings contrast somewhat with Majumdar and colleagues in that over 96% of our sample were prescribed medications to treat stroke/cardiovascular risk more broadly, including multiple types of antihypertensive drugs, and close to 40% of our group (all with confirmed HTN at study screening) were normotensive by the time they participated in study baseline evaluation. It is possible that individuals who are motivated to participate in a research study might also be more motivated to seek and obtain treatment for HTN and stroke risk than the general population of Ugandans.
Our results also found that even with a confirmed diagnosis of HTN and being prescribed cardiovascular risk reduction medications, BP control remained suboptimal for the majority of study participants with ESC-ESH HTN grades 1, 2 and 3 found in 83 (33.6%), 47 (19.0%) and 24 (9.7%) of our sample, respectively. This is consistent with other reports that suggest that despite the availability of advanced diagnostic options and multiple therapeutic drugs, suboptimal BP control is common among rural and urban SSA populations [22-24]. Among the ESC-ESH grades, there were few significant differences except that having diabetes, being sedentary, and being a smoker were associated with likelihood of worse BP control. There is a substantial overlap between etiology of HTN and diabetes because of their common metabolic pathways and shared risk factors [25]. Other reports from SSA have found strong associations between having HTN and diabetes [26]. Other reports from SSA have also identified sedentary lifestyle and smoking as HTN risk factors [27, 28], and the presence of each of these stroke risk factors may make it harder to achieve normal BP among those with HTN. It is noteworthy that individuals who were smokers or had problem alcohol use represented a relatively small minority of the total sample.
It must be noted that the group overall, was relatively young, with a mean age of approximately 55 years. It is possible that young individuals who have experienced stroke may be subsequently able to make changes to their lifestyle and health management that lead to positive downstream effects on BP and other health metrics. Another counterintuitive finding was that married individuals tended to have higher SBPs and higher ESC-ESH grades. While marriage is often used as a proxy marker of positive psychosocial support, it is possible that this is too simplistic of a conclusion and relationship dynamics such as disability and gender role expectations post-stroke could be impacting health and health management in other ways. Our findings suggest that social, community and family attitudes are likely important to stroke recovery and overall stroke risk reduction.
While our study had a number of strengths including a well-defined research sample, focus on individuals at relatively high risk for stroke, and a good representation of rural, suburban and urban participants, there are also some notable limitations. Individuals who agree to be in a clinical trial may be more motivated to adhere to stroke risk reduction treatments (including taking medication treatments for HTN) than the general population. While our study enrolled participants from three geographic locations in Uganda, it may still not represent the full population which includes many sub-groups of different tribal origin. The larger randomized controlled trial, from which this baseline data analysis is derived, is intended to focus on individuals who may have ongoing difficulties controlling BP for a variety of reasons, including lifestyle issues, suboptimal adherence to prescribed HTN medications, suboptimal management of comorbid conditions and/or not being prescribed the appropriate dosage or type of medication for HTN. The intervention that is being tested in the randomized trial from which the data were derived provides support for healthy lifestyle, adherence promotion, managing comorbidities, and communicating with healthcare providers to accurately monitor BP and response to medication. Knowing one is being monitored usually promotes adherence/care engagement even if temporarily. Our sample may not thus be generalizable to the full range of Ugandans with HTN. Finally, the clinical trial was largely conducted during the COVID-19 pandemic, and it is not clear how much of an impact this may have had on the types of participants who agreed to enroll in the study and/or their health behaviors during a global health crisis.
In conclusion, to help reduce the stroke burden in Uganda, our findings support the importance of raising awareness of HTN and helping individuals to manage their HTN and cardiovascular risk with both medications and lifestyle approaches. Policy efforts such as stroke education, HTN screening, and the need to be adherent with medications to manage HTN may help reduce the burden of stroke in Uganda and SSA more broadly.
Acknowledgments
The authors would like to thank the study participants for participating in this study.
Financial Disclosure
Research reported in this publication was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under Award Number R01NS118544. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
The authors declare that they have no competing interests.
Informed Consent
Written informed consent was obtained from all participants or their caregivers to participate in the study.
Author Contributions
MS, ETK, and MK conceived the study idea. SNM, MK, JN, DB, CC, LM, JNN, SM, CJB, JY, MS, ETK, and MK contributed to the research design and participated in data collection, management, analysis, and interpretation; writing of the report; and the decision to submit the report for publication. MS, CJB, JY, and MK wrote the first draft of the manuscript. All authors read and approved the final manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- WHO. Disease control priorities related to mental, neurological, developmental and substance abuse disorders. 2006; Geneva, Switzerland.
- WHO. Global status report on noncommunicable diseases. 2010. 2011.
- Agyemang C. Rural and urban differences in blood pressure and hypertension in Ghana, West Africa. Public Health. 2006;120(6):525-533.
doi pubmed - Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, Moran AE, et al. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2014;383(9913):245-254.
doi pubmed - Lemogoum D, Degaute JP, Bovet P. Stroke prevention, treatment, and rehabilitation in sub-saharan Africa. Am J Prev Med. 2005;29(5 Suppl 1):95-101.
doi pubmed - Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies C. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903-1913.
doi pubmed - Neal B, MacMahon S, Chapman N, Blood Pressure Lowering Treatment Trialists C. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure-lowering drugs: results of prospectively designed overviews of randomised trials. Blood Pressure Lowering Treatment Trialists' Collaboration. Lancet. 2000;356(9246):1955-1964.
doi pubmed - Wamala JF, Karyabakabo Z, Ndungutse D, Guwatudde D. Prevalence factors associated with hypertension in Rukungiri district, Uganda—a community-based study. Afr Health Sci. 2009;9(3):153-160.
pubmed - Sarfo FS, Treiber F, Jenkins C, Patel S, Gebregziabher M, Singh A, Sarfo-Kantanka O, et al. Phone-based Intervention under Nurse Guidance after Stroke (PINGS): study protocol for a randomized controlled trial. Trials. 2016;17(1):436.
doi pubmed - Kaddumukasa M, Kayima J, Kaddumukasa MN, Ddumba E, Mugenyi L, Pundik S, Furlan AJ, et al. Knowledge, attitudes and perceptions of stroke: a cross-sectional survey in rural and urban Uganda. BMC Res Notes. 2015;8:819.
doi pubmed - Kaddumukasa M, Najjuma J, Mbalinda SN, Kaddumukasa MN, Nakibuuka J, Burant C, Moore S, et al. Reducing stroke burden through a targeted self-management intervention for reducing stroke risk factors in high-risk Ugandans: A protocol for a randomized controlled trial. PLoS One. 2021;16(6):e0251662.
doi pubmed - Gurpreet K, Tee GH, Karuthan C. Evaluation of the accuracy of the Omron HEM-907 blood pressure device. Med J Malaysia. 2008;63(3):239-243.
pubmed - Ramzy I. Definition of hypertension and pressure goals during treatment (ESC-ESH Guidelines 2018). E-Journal of Cardiology Practice. 2019;17(18).
- Prevention C.f.D.C.a. Global Tobacco Surveillance System Data (GTSSData). 26-4-2023 [cited 2024]. Available from: https://www.cdc.gov/tobacco/global/gtss/gtssdata/index.html.
- WHO. International guide for monitoring alcohol consumption and related harm. [cited 2011]. Available from: http://apps.who.int/iris/bitstream/10665/66529/1/WHO_MSD_MSB_00.4.pdf.
- WHO. WHO STEPS manual, STEPS instrument. [cited 2011] Available from: http://www.who.int/chp/steps/STEPS_Manual.pdf?ua=1.
- Babor TF, et al. AUDIT: the alcohol use disorders identification test guidelines for use in primary care. 2001. World Health Organization.
- WHO. Global physical activity surveillance. Available from: http://www.who.int/chp/steps/GPAQ/en/.
- Majumdar U, Nanyonga Clarke R, Moran AE, Doupe P, Gadikota-Klumpers DD, Gidio A, Ssentamu D, et al. Hypertension screening, prevalence, treatment, and control at a large private hospital in Kampala, Uganda: A retrospective analysis. PLOS Glob Public Health. 2022;2(5):e0000386.
doi pubmed - Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, Chen J, et al. Global Disparities of Hypertension Prevalence and Control: A Systematic Analysis of Population-Based Studies From 90 Countries. Circulation. 2016;134(6):441-450.
doi pubmed - Ma J, Stafford RS. Screening, treatment, and control of hypertension in US private physician offices, 2003-2004. Hypertension. 2008;51(5):1275-1281.
doi pubmed - Adebolu FA, Naidoo M. Blood pressure control amongst patients living with hypertension presenting to an urban district hospital outpatient clinic in Kwazulu-Natal. Afr J Prim Health Care Fam Med. 2014;6(1):E1-6.
doi pubmed - Dennison CR, Peer N, Steyn K, Levitt NS, Hill MN. Determinants of hypertension care and control among peri-urban Black South Africans: the HiHi study. Ethn Dis. 2007;17(3):484-491.
pubmed - Duncan P, et al. Determinants of blood pressure control in rural KwaZulu-Natal, South Africa. South African Family Practice. 2014;56(6):297-304.
- Cheung BM, Li C. Diabetes and hypertension: is there a common metabolic pathway? Curr Atheroscler Rep. 2012;14(2):160-166.
doi pubmed - Adeniyi OV, Yogeswaran P, Longo-Mbenza B, Ter Goon D. Uncontrolled Hypertension and Its Determinants in Patients with Concomitant Type 2 Diabetes Mellitus (T2DM) in Rural South Africa. PLoS One. 2016;11(3):e0150033.
doi pubmed - Twinamasiko B, Lukenge E, Nabawanga S, Nansalire W, Kobusingye L, Ruzaaza G, Bajunirwe F. Sedentary Lifestyle and Hypertension in a Periurban Area of Mbarara, South Western Uganda: A Population Based Cross Sectional Survey. Int J Hypertens. 2018;2018:8253948.
doi pubmed - Walekhwa SN, Kisa A. Tobacco Use and Risk Factors for Hypertensive Individuals in Kenya. Healthcare (Basel). 2021;9(5):591.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
