| Journal of Neurology Research, ISSN 1923-2845 print, 1923-2853 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Neurol Res and Elmer Press Inc |
| Journal website https://www.neurores.org |
Review
Volume 12, Number 2, August 2022, pages 43-53
Ways of Knowing of the Brain and Mind: A Scoping Review of the Literature About Global Indigenous Perspectives
Louise Hardinga, b , Caterina J. Marraa, Vyshnavi Manoharaa, Judy Illesa, b
aNeuroethics Canada, Division of Neurology, Department of Medicine, University of British Columbia, Vancouver, BC, Canada
bCorresponding Author: Louise Harding and Judy Illes, Neuroethics Canada, Division of Neurology, Department of Medicine, University of British Columbia, Vancouver, BC, Canadaand
Manuscript submitted October 5, 2021, accepted December 7, 2021, published online February 24, 2022
Short title: Brain and Mind: A Scoping Review
doi: https://doi.org/10.14740/jnr708
- Abstract
- Introduction
- The Right to Inclusivity
- Methods
- Results
- Discussion
- Overall Conclusions and Recommendations
- References
| Abstract | ▴Top |
Indigenous peoples’ pursuit of brain health has been challenged by the violation of their rights to practice their cultures, speak their languages, and engage in traditional medical practices. Despite ongoing systemic oppression, indigenous knowledges and healing practices endure today and contribute to global understandings of the brain and mind. We conducted a scoping review of the academic literature, both research and reviews, which has examined the perspectives of global Indigenous people relevant to the neurological sciences. We searched three academic databases using phrases and terms pertaining to brain, neuro, mind, and Indigenous populations. Of the 66 articles included for analysis, 46 were research and 20 reviews or commentaries. The earliest date of publication was 1963; the majority were published after 2000. Most research studies involved consultations through focus groups or interviews, and involved people spanning all age groups. Sixty Indigenous communities were identified in the articles across 21 countries and regions and five continents. By contrast, the countries of affiliation of the corresponding authors were far less diverse: two-thirds were affiliated with institutions in the USA, Canada, Australia, or New Zealand. Only seven authors were in Latin America or Asia, and there were no corresponding authors primarily affiliated with institutions in Africa. The most prevalent focus of the articles was on mental health and illness, followed by aging and dementia. Ethics topics were embedded in two-thirds of articles, with substantial coverage of issues pertaining to public policy and public health, and cultural diversity and heterogeneity. The concepts of wellness and well-being, spirituality, holism and relationality were prominent reference features of this diverse body of research. This work supports the meaningful incorporation of Indigenous knowledges into initiatives involving the neurological sciences, such as the International Brain Initiative, the Canadian Brain Research Strategy, and the USA NIH BRAIN 2.0. Research with Indigenous populations that is collaborative and situates ethics at its core is key to the realization of a truly global, collaborative neuroscience.
Keywords: Brain; Mind; Indigenous peoples; Indigenous health; Ethics; Mental illness; Neurologic conditions; Wellness
| Introduction | ▴Top |
Civilizations around the world have long thought philosophically about the nature of the human mind and brain, and attempted, with varied success, to alleviate the unbearable suffering that can arise from brain and mental health disorders. While the emergence of the neurological sciences in the 20th century has drawn upon knowledge from diverse cultures and communities, Euro-Western biomedical frameworks for understanding the brain have come to largely dominate global approaches to brain research and clinical care.
Recently, extraordinary momentum in the field of neuroscience has been channeled into the establishment of large-scale, multinational brain initiatives coordinated by the International Brain Initiative (www.internationalbraininitiative.org) [1], involving Canada [2], the USA [3], Europe [4], Australia [5], Japan [6], South Korea [7] and China [8]. While this movement has called for a global collaborative neuroscience [9, 1], the epistemologies of Indigenous and other medically underserved and culturally diverse populations have yet to be fully developed within these endeavours. This gap may perpetuate the notion that neuroscience is culture-free and constrains the potential positive impact of these initiatives on diverse patient communities. In addition, it may hinder sharing of advances in neuroscience knowledge between and about communities that have radically different ways of thinking and knowing about the brain and mind.
| The Right to Inclusivity | ▴Top |
Indigenous peoples’ pursuit of brain health has been challenged by the violation of their rights to practice their cultures, speak their languages, and engage in traditional medical practices, among other rights. While there has been progress in the recognition of the rights of Indigenous peoples in recent decades through legislation, grassroots movements, and the establishment of the United Nations, the full impact of recent initiatives such as the 2007 United Nations Declaration on the Rights of Indigenous Peoples (UNDRIP) remains to be seen. Summarized in the words of the late Indigenous political leader Arthur Manuel, “Indigenous peoples’ poverty is not an accident, the result of our incompetence or bad luck, it is intentional and systematic” [10].
Despite ongoing systemic oppression, Indigenous knowledges and healing practices endure today and contribute to the resilience of communities and to global understandings and approaches to health and wellness. In Canada where our team of settler and Indigenous neuroethics researchers is located, Indigenous-led movements have become an important feature of the healthcare landscape through engaging diverse stakeholders to achieve community-identified goals [11]. Cross-cultural work by our team with the Tahltan First Nation in northern British Columbia surrounding genetic testing for early-onset familial Alzheimer’s disease (EOFAD) provided an example of how consideration of traditional knowledge and biomedical explanations of disease can together provide meaningful engagement with brain health care. It also called attention to the need to broaden Euro-Western research ethics for health research with Indigenous populations [12, 13].
Indigenous peoples’ perspectives on the brain and mind are exceptionally diverse, as is the body of research that has sought to understand these perspectives. Here we explored trends and themes within this literature to inform neuroscience initiatives and contribute towards the realization of a truly collaborative neuroscience.
| Methods | ▴Top |
Research question
The unifying research question for this work is: What are the defining themes of academic research about global Indigenous populations’ perspectives on the mind and brain?
We adapted the Joanna Briggs Institute (JBI) scoping review methodology described by Peters et al to answer this central question [14]. The methodological strategy is ideally suited to address broad research questions that are expected to have multiple and diverse contributing factors.
Statement of positionality and community engagement
This scoping review informs two larger projects in which the authors are engaged: a community-based project examining the meaning of brain wellness in an Indigenous health context, and the developing Indigenous initiatives of the Canadian Brain Research Strategy. Three of the authors (LH, VM and JI) identify as settlers; one author (CM) is a member of the Musqueam First Nation.
Definitions
We identified Indigenous peoples according to criteria provided by the United Nations: “(…) an Indigenous person self-identifies as Indigenous; has historical continuity with pre-colonial society; has a strong link to territory and natural resources; has a distinct social, economic, or political system; has a distinct language, culture, and/or belief system; forms a non-dominant societal group; and/or resolves to maintain and reproduce their ancestral environments and systems as distinctive peoples and societies” [15].
Search strategy
As per JBI protocol, we confirmed that there were no previous or ongoing registered literature review protocols on our topic by searching the PROSPERO International Prospective Register of Systematic Reviews and the JBI Register for Systematic Reviews. We therefore proceeded to identify relevant terms, subject headings, and databases for the search strategy of this study by reviewing the literature from a range of academic databases and consulting with the university health reference librarian. We focused on terms pertaining to the brain, mind and neuro to explore how they are used in the literature about Indigenous peoples (Supplementary Material 1, www.neurores.org). We attended carefully to the challenges of developing a comprehensive literature search strategy about Indigenous populations, as described in a parallel study [16]. The four databases we chose gave us access to contemporary and historical records about health and Indigenous populations: the Cumulative Index to Nursing and Allied Health Literature (CINAHL Complete: EBSCO, 1982 to present), MEDLINE (Ovid, 1982 to present), the Native Health Database (1652 to present), and Informit Indigenous Collections (1977 to present).
We conducted the search between June 17 and June 30, 2020. Citations were uploaded to Covidence (www.covidence.org) that automatically removes duplicate articles. Articles were screened for inclusion by at least two independent reviewers in two phases: titles and abstracts and then full-texts. All co-authors participated in the process of collecting data pertaining to the research question from the final set of included articles using an iteratively refined data extraction form (Supplementary Material 2, www.neurores.org). Co-authors LH and JI undertook final decision-making where needed.
We included academic journal articles about the opinions, beliefs, views and attitudes of any Indigenous individual or community about the brain, mind, or any brain or mind condition, disorder, or disease. For feasibility, we only reviewed articles with titles and abstracts written in English. For full-texts not written in English, we recruited translators fluent in those languages. Articles were excluded if they were out of scope, were not journal articles, or were written in a language for which translation was not available.
Data extraction and content analysis
We collected data on years of publication, article type (research or review), methods, countries of affiliation of corresponding authors, names and countries of Indigenous communities, defining characteristics of the research participants (e.g., age, community roles), foci of the articles, and ethics content. We used conventional terminology from Western neurology and psychiatry (DSM-V) to identify brain conditions described in the papers and preserved information about Indigenous conditions verbatim to prevent misinterpretation. To identify discourse pertaining to ethics, broadly defined, we searched for a priori content relevant to research, biomedical or clinical ethics, public health, and Indigenous ethics, and identified other emergent ethics content. We used a rich coding strategy to allow content to be assigned to more than one category (e.g., public health and policy; research ethics) as appropriate.
| Results | ▴Top |
Overarching features of the articles
A total of 66 articles met the final inclusion criteria (Fig. 1) [17]. Table 1 summarizes the overarching features of the final data set. The majority were written in English. Two-thirds were research (primary or secondary) and one-third were reviews (literature reviews and commentaries). The earliest date of publication was 1963, and there was a large increase in the number of publications around the turn of the millennium (Fig. 2).
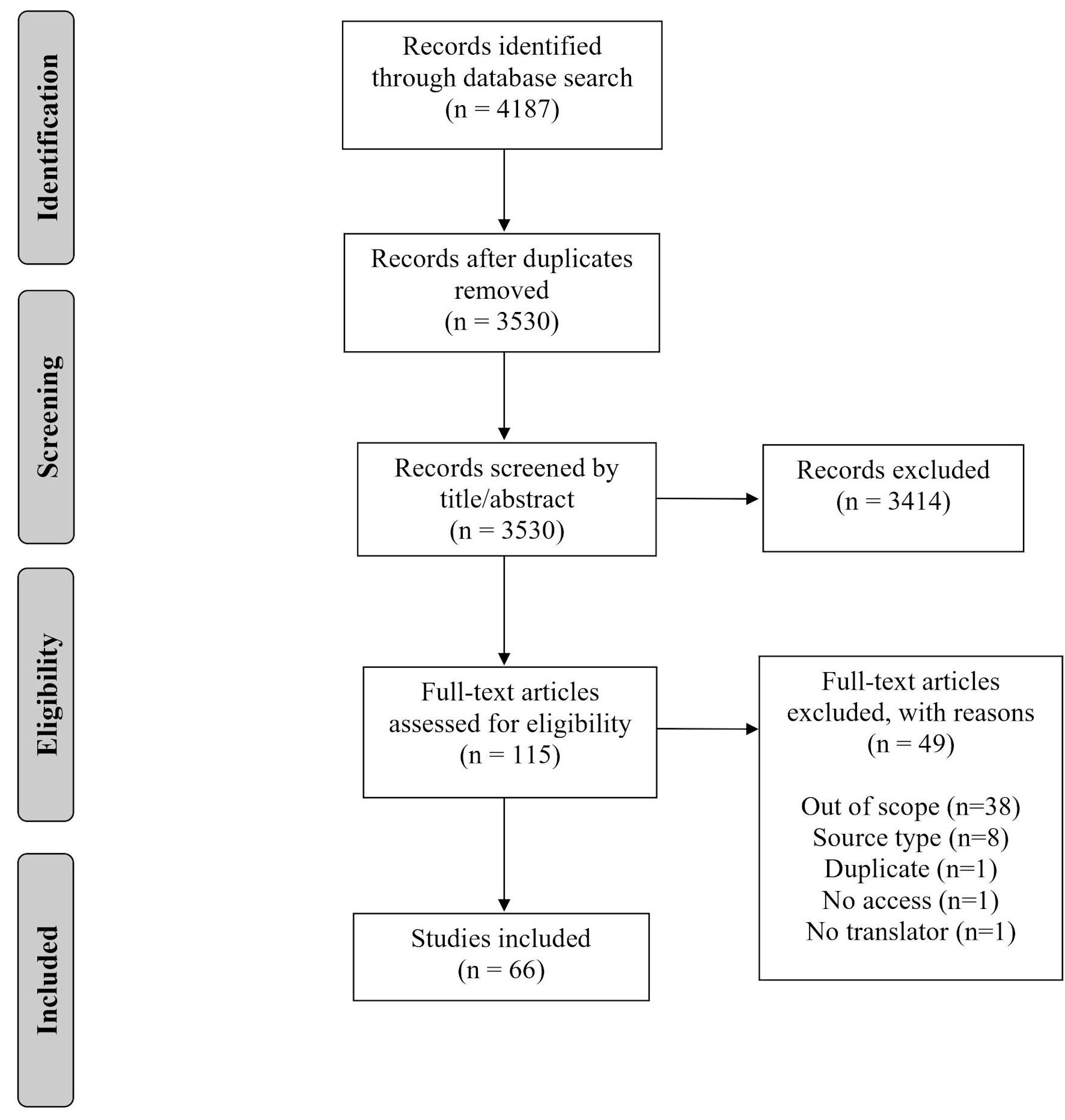 Click for large image | Figure 1. PRISMA flow diagram showing the process of inclusion of articles for the review [17]. PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses. |
 Click to view | Table 1. Overarching Features of the Dataset |
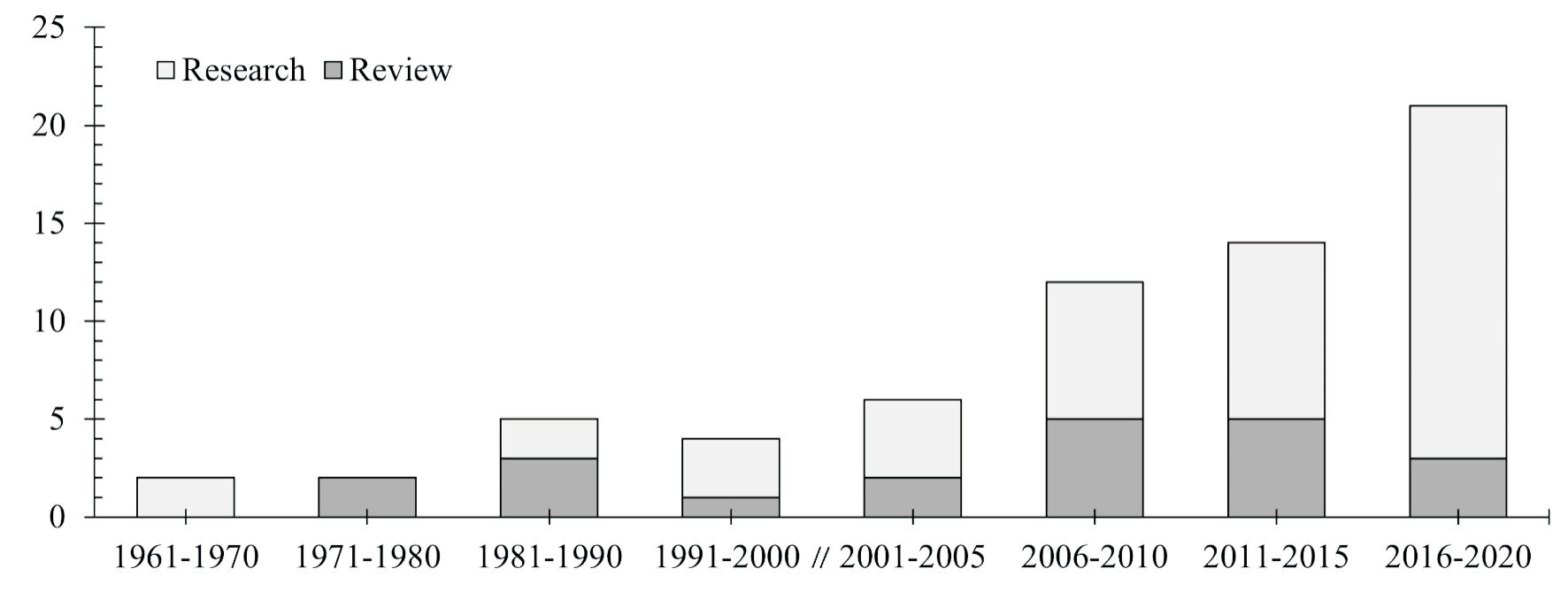 Click for large image | Figure 2. Years of publication of all articles (n = 66), separated by research and review. |
Two-thirds of the corresponding authors were affiliated primarily with institutions in the USA, Canada, Australia or New Zealand, and of the remaining five authors were in Latin American countries, five in Europe, and two in Asia. Corresponding authors in Canada and the USA were unique in that while most authors wrote primarily about local communities, authors from these two countries collectively wrote about Indigenous peoples living in 12 additional nations and regions around the world, primarily spanning South America and Mexico. For authors in the USA this was primarily through research; authors in Canada only discussed these countries in review articles.
Methods and participants
The majority (80%) of research studies involved some form of consultation with Indigenous peoples, most commonly as interviews or focus groups. A smaller portion of research articles used observational methods that involved field work in Indigenous communities (13%), two involved analyses of artwork, and one article examined cross-language differences in medical terminology. More than half (61%) of research studies were about adult populations. The next largest participant groups were healers (28%) and children and youth (22%). The majority (70%) of the review articles were commentaries or narratives, and there were three systematic reviews and three literature reviews.
Indigenous communities
We identified 66 highly diverse Indigenous groups in this body of research (Table 2 [13, 18-82]). Most were in North America (48%), while one-third (30%) were in Oceania, and one-fifth (19%) in South America (Fig. 3). Indigenous communities in Australia and the USA were a dominant focus, followed by Māori people in New Zealand and First Nations in Canada. There were only three articles about communities of each Asia and Africa, and no articles about the Indigenous peoples of Europe (e.g., Sámi of northern Europe, Inuit of Greenland).
 Click to view | Table 2. Indigenous Groups in the Articles Organized by Frequency |
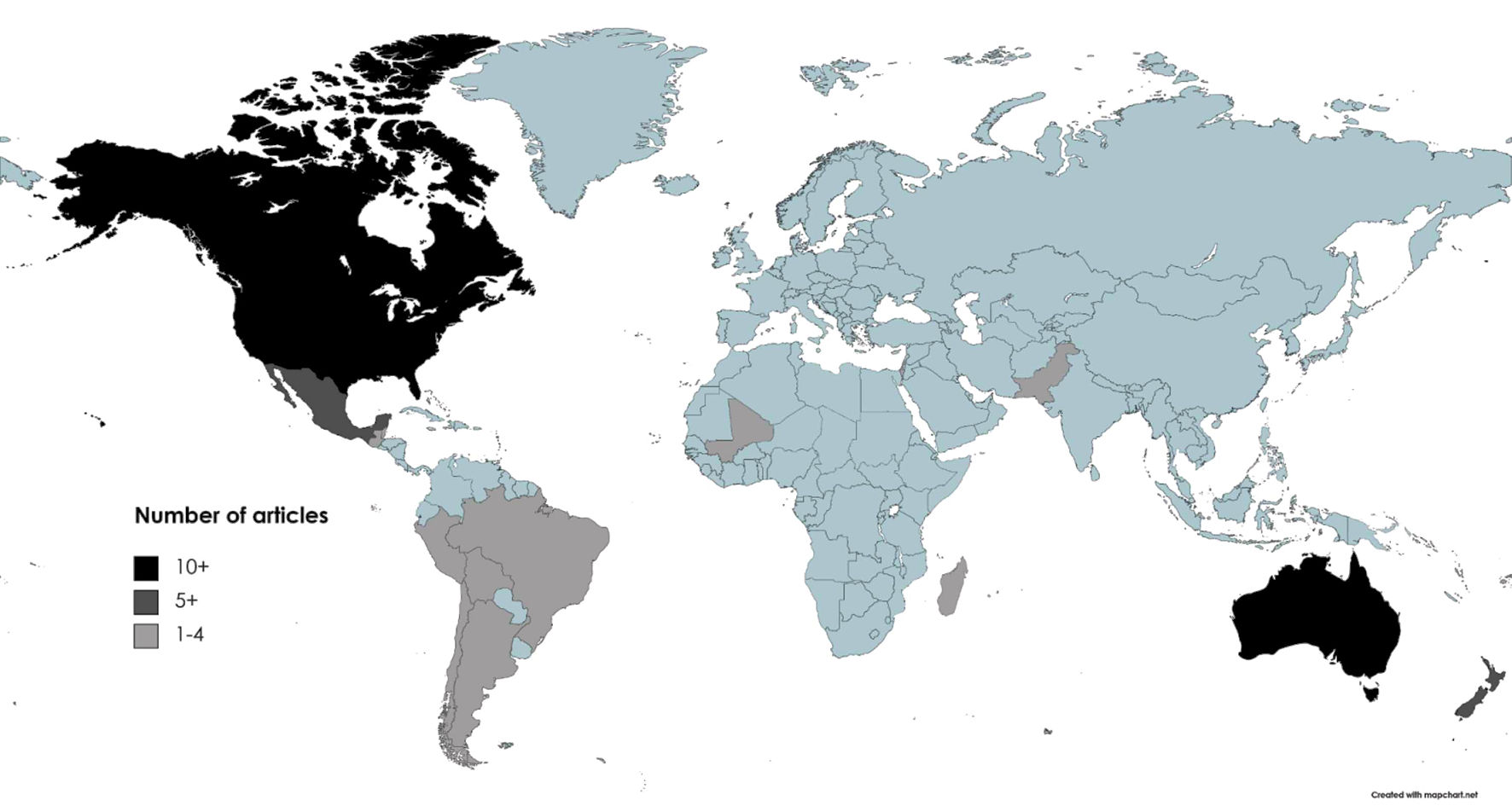 Click for large image | Figure 3. Number of total articles (n = 66) about Indigenous communities in countries around the world. |
The way that Indigenous communities were identified in the articles differed across continents and limited the number of distinct communities we could identify. Authors writing about Australia and South America mainly used broad group names (e.g., Indigenous peoples of Peru, Aboriginal people in Western Australia), while communities in North America were frequently identified by their specific nations (e.g., Cree, Penobscot).
Foci of the articles
Based on the content of the articles, we clustered main foci about brain conditions into four major categories: mental health (a focus of 42% of all articles), aging and dementia (20%), five subcategories within the category of non-aging-related conditions together comprising 18% of the total (traumatic brain injury, strokes and acquired communication disorders, headaches, movement disorders, epilepsy), and neurodevelopmental disorders (3%).
Mental illness was by far the greatest focus in the articles returned, variously describing this condition, for example, as “thinking too much”, “pain in the head”, “heat in the head”, “sadness of the soul”, “spoiled mind”, “crazy”, “anxiety”, “sick” or “lost mind”, “spirit possession” and “madness”. Addiction, trauma, psychotic experiences, schizophrenia, and emotions and psychopathology were also mentioned. In counterpart to mental illness, mental health was also described in terms of “wellness” and “well-being”. Mental health training using psychotherapy, cognitive behavioural therapy, neuropsychiatry, shamanic healing and Indigenous psychology were the interventions reported in the dataset.
Dementia was another focus of the articles. The terms aging, cognitive decline, and Alzheimer’s were used interchangeably to describe this condition. This theme was only a major focus in articles about Indigenous communities in Australia, Canada and the USA, while mental health was a focus of articles about a much broader range of countries. In the category of non-aging-related brain conditions, articles pertaining to brain injury and concussion were most frequent. We noted two articles on headaches and two on epilepsy in the dataset, as well as one on a movement disorder (Machado-Joseph Disease). Where articles focused on a mixture of neurologic and mental health conditions, aging, headaches, psychosis, and neuromuscular symptoms were the foci. Three articles focused on physical pain; one related to cancer. Of the two that focused on neurodevelopmental disorders, one focused on autism and the other on fetal alcohol spectrum disorder.
The fifth category of studies, cross-cultural analyses aimed at understanding differences in how Indigenous peoples think and reason, accounted for 5% of articles. Two of the articles were published by a single research team in the same year and pertained to moral judgement and perceptions about the mind among iTaukei Fijians [18, 19]. The third was about the development of a paradigm to describe the “Indigenous Mind” in an Australian context: “I see Indigenous Mind as an attempt to de-colonise the thought processes of Indigenous Australians and retrain them to go back to our cultural and spiritual base. To see, believe and interpret the world and everything in it through our cultural mind, our pina kuru. It is an attempt to stop the poison of mental colonialism (white way of thinking) contaminating our culture, our spirituality our consciousness, our psyche” [20].
In a specific analysis of the articles written by authors affiliated with institutions in Canada, where our research team is located, there was a two-fold focus on dementia and aging over the sample: this theme accounted for almost half (42%) of all articles from Canada. Mental health was an equally large focus in these articles over the total sample (42%). Two out of the total four articles about brain injury were from research teams in Canada and investigated perceptions and knowledge among several First Nations communities in Ontario.
Ethics content
We derived seven categories of ethics content from the two-thirds of articles that contained it: public policy/public health (discussed in 39% of all articles), importance of cultural identity and heterogeneity of multicultural groups (21%); research ethics (8%); access to services and resource allocation (6%); the impacts of contact with White civilizations and colonization on health and culture (3%); and locus of caregiving and decision-making (2%).
Public health and policy dominated the papers when observed through the ethics lens. These quotes capture the essence of the overwhelming theme: “Western cultures … have historically denied Indigenous peoples and people with disabilities their human rights to self-determination, disabling both groups” [21].
“Indigenous community leadership and participation is a key factor to Indigenous health program success. Community is extremely important to First Nations peoples. Therefore, health interventions with First Nations must focus on collaboration with community members and be guided by culture” [22].
A central theme of cultural awareness and diversity was also a significant focus. Papers discussed maintaining uniqueness and cultural identity, preservation of traditional knowledge while appreciating collective values, two-eyed seeing in the context, for example of bioculturalism [23], cultural training of health care providers, and appreciation of cultural views of mind: “Whether we looked at how concepts of minds are structured or how these structures are used to predict other variables, cultural differences mattered. Much more cross-cultural work is needed before we can confidently make any universal claims about how humans conceive of minds, and more attention needs to be paid to specific historical differences in cultural context” [19].
Of the few papers with research ethics content, researcher bias and positionality, mindset, self-reflection, and community engagement were the themes. Rituals of gift- and tobacco-giving were discussed once. The irrelevance of the process of Western approaches to consent in another: “These elders found the usual research format of consent forms, confidentiality, and data collection highly amusing, and as one said, he ‘would never participate in such nonsense.’ Nevertheless, they humored me by signing consent for participation in an ethics committee-approved interview study. They considered themselves to be my teachers and were satisfied when I could repeat back what they had said correctly” [24].
| Discussion | ▴Top |
Neuroscience initiatives must embrace the perspectives of the diverse communities they strive to benefit to truly meet the goal of global collaboration. In this scoping review of 66 academic articles about global Indigenous peoples’ perspectives on the brain and mind we located a heterogenous body of literature to which neuroscientists can refer to incorporate these perspectives into their work. Several key features of this literature distinguish it from the biomedical models of disease, healing, and treatment that dominate neuroscience research and clinical practice.
The first reference feature of this work is the holistic view on brain health and significant focus on mental wellness. While the foci of the articles spanned major neurologic, mental health and other conditions familiar to biomedical communities, notions of the mind, wellness/well-being, spirituality and relationships were woven throughout. Concepts of wellness often included considerations of family, community and society more broadly, as was described by Watts, who explored substance dependency and recovery: “The Healing Forest program starts with the premise that an ailing individual tree, once healed and returned to a forest where the soil remains diseased, will become diseased again itself. A forest cannot heal unless harmful elements present in its soil are removed and replaced with healthy elements” [25].
Spiritual elements of well-being were also prevalent in descriptions of the etiology, classification and treatment of various disturbances and illnesses: “Spirituality is acknowledged by many Indigenous people to be the strengthening foundation of all of the domains of (social and emotional wellbeing), of a ‘deep wellbeing’ (Grieves, 2006, p. 52) and the source of healing” [26].
A second defining feature of this literature is the unique ethics themes. Incorporating considerations including culture, colonization, and access are crucial to the collaborative way forward for neuroscience that we are envisioning and were described in a significant portion of the literature. Less prevalent in the literature we found, though of critical importance, was Indigenous research ethics. For example, many articles lacked statements by the authors that indicated their positionality and relationship relative to the Indigenous communities they studied. As described through the principles of OCAP® (The First Nations principles of ownership, control, access, and possession) that are regarded as the minimum standard for research with First Nations peoples in Canada together with Chapter 9 of the Tri-Council Policy Statement 2 (TCPS 2), ownership, control, access, and possession are essential (https://fnigc.ca/ocap-training/; [83]). As such, impactful and respectful research with Indigenous populations must involve deep, meaningful collaboration: “(…) the larger project to recover (historically subjugated) Indigenous knowledges will not succeed in influencing scholars and professionals in psychology absent processes of robust community engagement” [27].
A promising feature of the body of literature we studied was the increasing publication trend over time that may be taken as proxy measure of a growing interest and motivation within academia to understand and incorporate Indigenous perspectives. The increase started close to the millennium and may be associated with the global Indigenous rights movement catalyzed by the United Nations in the 1980s and recognized in the UNDRIP in 2007.
Limitations
The literature we located was mainly about Indigenous communities in the Americas and Oceania, which limits applicability to populations in Africa and Asia. There were few corresponding authors outside of Canada, USA, Australia, and New Zealand. This limitation may reflect a need for more scholarship led by authors and institutions in underresourced countries, the constraints of the methods and global reach of the databases searched [84], the exclusion of non-English language titles and abstracts, or a combination of these phenomena.
Our decision to focus on Indigenous groups globally was based on the articulation of their shared rights in UNDRIP, but the importance of the specificity and distinctiveness of individual communities cannot be overemphasized. Similarly, there is diversity within Euro-Western biomedical understandings of the brain. It is not our intention to fabricate a binary distinction per se between these two knowledge systems. The scoping review methodology focuses on commonalities and generalizations; the ability to provide in depth analyses of content is necessarily limited.
Finally, the scope of the literature was limited by the choice of general search terms in the neurological sciences. Other research about specific brain diseases and mental health conditions can be located using different subject headings and keywords.
| Overall Conclusions and Recommendations | ▴Top |
Understanding Indigenous peoples’ perspectives on brain health can contribute to wellness targets and to human rights while also expanding the scope and reach of neuroscience. These efforts must involve meaningful collaboration with Indigenous communities and hold ethics at the center. This scoping review reveals and elaborates on Indigenous ways of knowing about health and how they can differ from Euro-Western biomedical understandings. We bring that knowledge here to focus on the global neurological sciences community through specific examples from the Indigenous academic literature. In our dataset, key reference features were the concepts of wellness and well-being, holism, the mind, spirituality, and relationality, as well as the unique ethics topics that pertain to Indigenous populations. Other important features were the substantial foci on mental health, aging and dementia, and an increase in publications starting at the turn of the millennium.
We identified few articles from corresponding authors affiliated outside of Canada, USA, Australia, and New Zealand. Corresponding authors in Canada and the USA collectively wrote about communities across 12 other countries and regions, with a focus on Mexico and South America. Because Indigenous groups residing in Canada and the USA were identified with a higher level of specificity than those in other countries, the dataset about perspectives on the brain and mind in this part of the world is more detailed than others.
An important focus for future work is the specific link between violence against Indigenous peoples (e.g., continued colonialism, violation of human rights, racism and other forms of discrimination) and brain wellness. As authors, we understand the primacy of this connection as a key motivation for all our work with Indigenous communities, and there is a well-developed body of literature on the link between these factors and Indigenous peoples’ health in general (e.g., [85, 86]). While an analysis of these connections is out of scope for the present review, a paper by Dudgeon et al that explores a decolonizing approach to psychology that encompasses how “the specific impact of colonisation has resulted in enduring forms of trauma which have harmed the mental and emotional health of Indigenous people in particular ways” [54], and more recently by Perreault et al [87], are particularly relevant.
This work supports the meaningful incorporation of Indigenous knowledges into multinational neuroscience initiatives and the neurological sciences more broadly. Based on the findings here, mental wellness and brain health for aging Indigenous populations may be two priority areas for future collaborative work. It is one step further in the continued movement toward a more inclusive and expansive approach to understanding and approaching the causes, prevention and treatment of illnesses affecting the brain and mind.
| Supplementary Material | ▴Top |
Suppl 1. Search strategies for all databases
Suppl 2. Data extraction chart
Acknowledgments
Neuroethics Canada is located on the traditional, ancestral, and unceded territory of the xʷməθkʷəỳəm (Musqueam people). We thank Dr. Malcolm King, an Indigenous health researcher and member of the Mississaugas of the Credit First Nation, for inspiring the idea for this project during a consultation in December 2019, Charlotte Beck for her assistance as a UBC health reference librarian, and members of Neuroethics Canada for providing their input and assistance at various stages of the research. We also sincerely acknowledge peer reviewers for their comments, and the valuable engagement with colleagues at the 2021 International Neuroethics Society Annual Meeting.
Financial Disclosure
This work was generously supported by the Canadian Brain Research Strategy (Canadian Institutes of Health Research, #171583; 03027 IC-127354 (JI, Co-Principal Investigator)), North Growth Foundation (JI), National Institute of Mental Health (JI; RF1#MH117805 01), a Canadian Institutes of Health Research Canada Graduate Scholarship Master’s Award (LH; #6556), and a W. Maurice Young Centre for Applied Ethics Graduate Fellowship (LH). JI is a University of British Columbia Distinguished University Scholar.
Conflict of Interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Author Contributions
LH and JI conceived of the presented work. LH, CM and JI collaborated on design of the work. All authors contributed to acquisition, analysis and interpretation of data, and to the drafting and revision of the manuscript including figures, tables and supplementary materials.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
EOFAD: early-onset familial Alzheimer’s disease; JBI: Joanna Briggs Institute; OCAP®: The First Nations principles of ownership, control, access, and possession; TCPS 2: Tri-Council Policy Statement 2; UNDRIP: United Nations Declaration on the Rights of Indigenous Peoples
| References | ▴Top |
- International Brain Initiative. International brain initiative: an innovative framework for coordinated global brain research efforts. Neuron. 2020;105(2):212-216.
doi pubmed - Illes J, Weiss S, Bains J, Chandler JA, Conrod P, De Koninck Y, Fellows LK, et al. A neuroethics backbone for the evolving Canadian brain research strategy. Neuron. 2019;101(3):370-374.
doi pubmed - Martin CL, Chun M. The BRAIN Initiative: Building, Strengthening, and Sustaining. Neuron. 2016;92(3):570-573.
doi pubmed - Salles A, Bjaalie JG, Evers K, Farisco M, Fothergill BT, Guerrero M, Maslen H, et al. The human brain project: responsible brain research for the benefit of society. Neuron. 2019;101(3):380-384.
doi pubmed - Australian Brain Alliance Steering Committee. Australian Brain Alliance. Neuron. 2016;92(3):597-600.
doi pubmed - Okano H, Sasaki E, Yamamori T, Iriki A, Shimogori T, Yamaguchi Y, Kasai K, et al. Brain/MINDS: a Japanese national brain project for marmoset neuroscience. Neuron. 2016;92(3):582-590.
doi pubmed - Jeong SJ, Lee H, Hur EM, Choe Y, Koo JW, Rah JC, Lee KJ, et al. Korea Brain Initiative: Integration and Control of Brain Functions. Neuron. 2016;92(3):607-611.
doi pubmed - Poo MM, Du JL, Ip NY, Xiong ZQ, Xu B, Tan T. China brain project: basic neuroscience, brain diseases, and brain-inspired computing. Neuron. 2016;92(3):591-596.
doi pubmed - Vogt N. Collaborative neuroscience. Nat Methods. 2020;17(1):22.
doi pubmed - Manuel A. Chapter 4: From dispossession to dependency. In: The reconciliation manifesto. Toronto: James Lorimer and Company, 2017; p. 70-71.
- Allen L, Hatala A, Ijaz S, Courchene ED, Bushie EB. Indigenous-led health care partnerships in Canada. CMAJ. 2020;192(9):E208-E216.
doi pubmed - Stevenson S, Beattie BL, Vedan R, Dwosh E, Bruce L, Illes J. Neuroethics, confidentiality, and a cultural imperative in early onset Alzheimer disease: a case study with a First Nation population. Philos Ethics Humanit Med. 2013;8:15.
doi pubmed - Cabrera LY, Beattie BL, Dwosh E, Illes J. Converging approaches to understanding early onset familial Alzheimer disease: A First Nation study. SAGE Open Med. 2015;3:2050312115621766.
doi pubmed - Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, McInerney P, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. 2020;18(10):2119-2126.
doi pubmed - Bishop-Williams KE, Sargeant JM, Berrang-Ford L, Edge VL, Cunsolo A, Harper SL. A protocol for a systematic literature review: comparing the impact of seasonal and meteorological parameters on acute respiratory infections in Indigenous and non-Indigenous peoples. Syst Rev. 2017;6(1):19.
doi pubmed - Harding L, Marra CJ, Illes J. Establishing a comprehensive search strategy for Indigenous health literature reviews. Syst Rev. 2021;10(1):115.
doi pubmed - Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. 2009;89(9):873-880.
doi pubmed - McNamara RA, Willard AK, Norenzayan A, Henrich J. Weighing outcome vs. intent across societies: How cultural models of mind shape moral reasoning. Cognition. 2019;182:95-108.
doi pubmed - Willard AK, McNamara RA. The minds of god(s) and humans: differences in mind perception in Fiji and North America. Cogn Sci. 2019;43(1):1-30.
doi pubmed - Reid J. Why Indigenous mind? Ngoonjook. 2004;25:34-39.
doi - Kapp SK. Navajo and autism: The beauty of harmony. Disabil Soc. 2011;26(5):583-595.
doi - Hunt C, Michalak A, Lefkimmiatis C, Johnston E, Macumber L, Jocko T, Ouchterlony D. Exploring concussion awareness in hockey with a First Nations community in Canada. Public Health Nurs. 2018;35(3):202-210.
doi pubmed - Henderson JN, Traphagan JW. Cultural factors in dementia: perspectives from the anthropology of aging. Alzheimer Dis Assoc Disord. 2005;19(4):272-274.
doi pubmed - Mehl-Madrona L. What traditional indigenous elders say about cross-cultural mental health training. Explore (NY). 2009;5(1):20-29.
doi pubmed - Watts LK. Applying a cultural models approach to American Indian substance dependency research. Am Indian Alsk Native Ment Health Res. 2001;10(1):34-50.
doi pubmed - Dudgeon P, Kelly K. Contextual factors for research on psychological therapies for Aboriginal Australians. Aust Psychol. 2014;49(1):8-13.
doi - Gone JP. "The thing happened as he wished": recovering an American Indian cultural psychology. Am J Community Psychol. 2019;64(1-2):172-184.
doi pubmed - BigFoot DS, Schmidt SR. Honoring children, mending the circle: cultural adaptation of trauma-focused cognitive-behavioral therapy for American Indian and Alaska native children. J Clin Psychol. 2010;66(8):847-856.
doi pubmed - Cipriani G, Borin G. Understanding dementia in the sociocultural context: a review. Int J Soc Psychiatry. 2015;61(2):198-204.
doi pubmed - Friedman DB, Laditka SB, Laditka JN, Wu B, Liu R, Price AE, Tseng W, et al. Ethnically diverse older adults' beliefs about staying mentally sharp. Int J Aging Hum Dev. 2011;73(1):27-52.
doi pubmed - Haozous EA, Doorenbos AZ, Stoner S. Pain management experiences and the acceptability of cognitive behavioral strategies among American Indians and Alaska Natives. J Transcult Nurs. 2016;27(3):233-240.
doi pubmed - Haozous EA, Knobf MT, Brant JM. Understanding the cancer pain experience in American Indians of the Northern Plains. Psychooncology. 2011;20(4):404-410.
doi pubmed - Hodge DR, Limb GE, Cross TL. Moving from colonization toward balance and harmony: a Native American perspective on wellness. Soc Work. 2009;54(3):211-219.
doi pubmed - Laditka SB, Laditka JN, Liu R, Price AE, Friedman DB, Wu B, Ivey SL. How do older people describe others with cognitive impairment? A multiethnic study in the United States. Ageing Soc. 2013;33(3):369-392.
doi - McCabe G. Mind, body, emotions and spirit: Reaching to the ancestors for healing. Couns Psychol Q. 2008;21(2);143-152.
doi - Yurkovich EE, Lattergrass I. Defining health and unhealthiness: Perceptions held by Native American Indians with persistent mental illness. Ment Health Relig Cult. 2008;11(5):437-459.
doi - Chandler M. The "Mental" Health of Canada's indigenous children and youth: finding new ways forward. Healthc Q. 2011;14(Spec No 2):50-57.
doi pubmed - Johnston K, Preston R, Strivens E, Qaloewai S, Larkins S. Understandings of dementia in low and middle income countries and amongst indigenous peoples: a systematic review and qualitative meta-synthesis. Aging Ment Health. 2020;24(8):1183-1195.
doi pubmed - Keightley ML, King GE, Jang SH, White RJ, Colantonio A, Minore JB, Katt MV, et al. Brain injury from a first nations' perspective: teachings from elders and traditional healers. Can J Occup Ther. 2011;78(4):237-245.
doi pubmed - McCabe GH. The healing path: A culture and community-derived indigenous therapy model. Psychotherapy (Chic). 2007;44(2):148-160.
doi pubmed - Webkamigad S, Cote-Meek S, Pianosi B, Jacklin K. Exploring the appropriateness of culturally safe dementia information with indigenous people in an Urban Northern Ontario Community. Can J Aging. 2020;39(2):235-246.
doi pubmed - Lanting S, Crossley M, Morgan D, Cammer A. Aboriginal experiences of aging and dementia in a context of sociocultural change: qualitative analysis of key informant group interviews with Aboriginal seniors. J Cross Cult Gerontol. 2011;26(1):103-117.
doi pubmed - Cornect-Benoit A, Pitawanakwat K, Wiikwemkoong Unceded Territory Collaborating First Nation C, Walker J, Manitowabi D, Jacklin K. Nurturing meaningful intergenerational social engagements to support healthy brain aging for Anishinaabe older adults. Can J Aging. 2020;39(2):263-283.
doi pubmed - Pudenz RH. Aztec medicine with comments on Mexican neurosurgery. Ariz Med. 1971;28(7):503-508.
- Wilson J, Sabo S, Chief C, Clark H, Yazzie A, Nahee J, Leischow S, et al. Dine (Navajo) healer perspectives on commercial tobacco use in ceremonial settings: an oral story project to promote smoke-free life. Am Indian Alsk Native Ment Health Res. 2019;26(1):63-78.
doi pubmed - Hammerschlag CA. The Huichol offering: a shamanic healing journey. J Relig Health. 2009;48(2):246-258.
doi pubmed - Tousignant M. [Emotions and psychopathology: an indigenous theory]. Acta Psiquiatr Psicol Am Lat. 1981;27(3):194-199.
- Whealin JM, Yoneda AC, Nelson D, Hilmes TS, Kawasaki MM, Yan OH. A culturally adapted family intervention for rural Pacific Island veterans with PTSD. Psychol Serv. 2017;14(3):295-306.
doi pubmed - Arkles R, Jankelson C, Radford K, Jackson Pulver L. Family caregiving for older Aboriginal people in urban Australia: Disclosing worlds of meaning in the dementia experience. Dementia (London). 2020;19(2):397-415.
doi pubmed - Armstrong E, Coffin J, Hersh D, Katzenellenbogen JM, Thompson SC, Ciccone N, Flicker L, et al. "You felt like a prisoner in your own self, trapped": the experiences of Aboriginal people with acquired communication disorders. Disabil Rehabil. 2021;43(13):1903-1916.
doi pubmed - Carr JJ, Lalara J, Lalara G, O'hare G, Massey L, Kenny N, Pope KE, et al. "Staying strong on the inside and outside" to keep walking and moving around: Perspectives from Aboriginal people with Machado Joseph Disease and their families from the Groote Eylandt Archipelago, Australia. PLoS One. 2019;14(3):1-17.
doi pubmed - Cawte JE. Australian ethnopsychiatry in the field: a sampling in North Kimberley. Med J Aust. 1964;1:467-472.
doi pubmed - Cawte J. Emic accounts of a mystery illness: the Groote Eylandt syndrome. Aust N Z J Psychiatry. 1984;18(2):179-187.
doi pubmed - Dudgeon P, Bray A, D'Costa B, Walker R. Decolonising psychology: Validating social and emotional wellbeing. Aust Psychol. 2017;52(4):316-325.
doi - Hamilton SL, Maslen S, Watkins R, Conigrave K, Freeman J, O'Donnell M, Mutch RC, et al. 'That thing in his head': Aboriginal and non-Aboriginal Australian caregiver responses to neurodevelopmental disability diagnoses. Sociol Health Illn. 2020;42(7):1581-1596.
doi pubmed - Kilcullen M, Swinbourne A, Cadet-James Y. Aboriginal and Torres Strait Islander health and well-being: Implications for a cognitive behavioural therapy framework. Aust Psychol. 2016;51(6):453-462.
doi - Pollitt PA. The problem of dementia in Australian aboriginal and Torres Strait Islander communities: an overview. Int J Geriatr Psychiatry. 1997;12(2):155-163.
doi - Coleman R, Sim G. The sacredness of the head: Cultural implications for neuroscience nurses. Australas J Nerosci. 2003;16(2):20-22.
- Corbett A, Francis K, Chapman Y. The experience of whanau caring for members disabled from the effects of a cerebro-vascular accident. Contemp Nurse. 2006;22(2):255-263.
doi pubmed - Elder H, Te Waka Kuaka, Te Waka Oranga. Working with Whanau to improve outcomes. Aust NZ Fam Ther. 2017;38(1):27-42.
doi - Lakhani A, Townsend C, Bishara J. Traumatic brain injury amongst indigenous people: a systematic review. Brain Inj. 2017;31(13-14):1718-1730.
doi pubmed - Mark GT, Lyons AC. Maori healers' views on wellbeing: the importance of mind, body, spirit, family and land. Soc Sci Med. 2010;70(11):1756-1764.
doi pubmed - Mark G, Lyons A. Conceptualizing mind, body, spirit interconnections through, and beyond, spiritual healing practices. Explore (NY). 2014;10(5):294-299.
doi pubmed - Taitimu M, Read J, McIntosh T. Nga Whakawhitinga (standing at the crossroads): How Maori understand what Western psychiatry calls "schizophrenia". Transcult Psychiatry. 2018;55(2):153-177.
doi pubmed - Torsch VL, Ma GX. Cross-cultural comparison of health perceptions, concerns, and coping strategies among Asian and Pacific Islander American elders. Qual Health Res. 2000;10(4):471-489.
doi pubmed - Dangatanga J. The Yolngu "headache". AborigIsl Health Work. 1982;6(1):21-24.
- Dobkin de Rios M. The vidente phenomenon in third world traditional healing: an Amazonian example. Med Anthropol. 1984;8(1):60-70.
doi pubmed - Villoldo A. Jaguar medicine. Altern Ther Health Med. 2007;13(5):14-16.
- Dorsher PT. The languages of healing: linked by a common thread. J Altern Complement Med. 2010;16(8):907-913.
doi pubmed - Roysircar G. American Indians and culturally sensitive therapy. J Multicult Couns Devel. 2012;40(2):66-69.
doi - Carod-Artal FJ, Vazquez-Cabrera C. [Neurological anthropology among the Kamayura Indians of the Alto Xingu]. Rev Neurol. 2001;32(7):688-695.
doi pubmed - Carod-Artal FJ, Vazquez-Cabrera CB. [Treatment of headaches among the Aborigines of Tierra de Fuego. A comparison with other anthropological studies]. Rev Neurol. 2008;47(7):374-379.
doi pubmed - Loizaga-Velder A, Verres R. Therapeutic effects of ritual ayahuasca use in the treatment of substance dependence—qualitative results. J Psychoactive Drugs. 2014;46(1):63-72.
doi pubmed - Carod-Artal FJ, Vazquez-Cabrera CB. [Ethnographic study of neurological and mental diseases among the Uru-Chipaya peoples of the Andean Altiplano]. Rev Neurol. 2005;41(2):115-125.
doi pubmed - Hatala AR, Waldram JB, Caal T. Narrative structures of maya mental disorders. Cult Med Psychiatry. 2015;39(3):449-486.
doi pubmed - Molina FC. La terminologianeuropsiquiatriaenelquechua del sieglo XVI. [Neuropsychiatry terminology in 16th century Quechua.] An Fac Med. 1963;46:277-299.
doi - Miletto G. Vuestraditionnelles sur l'epilepsie chez les dogons. [Traditional views on epilepsy among the Dogons.] Medecine Tropicale. 1981;41(3):291-297.
- Sharp LA. Exorcists, psychiatrists, and the problems of possession in northwest Madagascar. Soc Sci Med. 1994;38(4):525-542.
doi - Palgi P. Persistent traditional Yemenite ways of dealing with stress in Israel. Ment Health Soc. 1979;5(3-4):113-140.
- Choudhry FR, Khan TM, Park MS, Golden KJ. Mental health conceptualization and resilience factors in the Kalasha youth: an indigenous ethnic and religious minority community in Pakistan. Front Public Health. 2018;6:187.
doi pubmed - Carod FJ, Vazquez-Cabrera C. [A transcultural view of neurological and mental pathology in a Tzeltal Maya community of the Altos Chiapas]. Rev Neurol. 1996;24(131):848-854.
- Pace J. "Place-ing" dementia prevention and care in NunatuKavut, Labrador. Can J Aging. 2020;39(2):247-262.
doi pubmed - Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council of Canada, and Social Sciences and Humanities Research Council of Canada. Tri-Council policy statement: Ethical conduct for research involving humans. 2014.
- Aalai E, Gleghorn C, Webb A, Glover SW. Accessing public health information: a preliminary comparison of CABI's GLOBAL HEALTH database and MEDLINE. Health Info Libr J. 2009;26(1):56-62.
doi pubmed - Gracey M, King M. Indigenous health part 1: determinants and disease patterns. Lancet. 2009;374(9683):65-75.
doi - King M, Smith A, Gracey M. Indigenous health part 2: the underlying causes of the health gap. Lancet. 2009;374(9683):76-85.
doi - Perreault ML, King M, Gabel C, Mushquash CJ, De Koninck Y, Lawson A, Marra C, et al. An Indigenous Lens on Priorities for the Canadian Brain Research Strategy. Can J Neurol Sci. 2022:1-9.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Neurology Research is published by Elmer Press Inc.
